Children and Telehealth in Mental Healthcare: What We Have Learned From COVID‐19 and 40,000+ Sessions
Abstract
Objective
Of the many impacts of COVID‐19 on contemporary healthcare is the rapid and overwhelming shift to remote telehealth (TH) service. The precise effect of TH on treatment is yet unknown, and the possible child/adult differences are an essential point of clarification for the utility of TH services and efforts to improve upon them.
Methods
The current study considers data reflecting pre‐, during‐, and post‐COVID‐19 lockdown over the first six months of 2020. Data comprise records of N = 43,294 services delivered to N = 2520 unique clients across multiple outpatient mental health sites at a Certified Community Based Mental Health Clinic (CCBHC) in Rockland County, NY, an area hard hit by COVID‐19.
Results
Results demonstrate significant differences between child and adult sessions with a relative decrease in the number of child mental health services with the switch to TH in March 2020 (onset of lockdown) and a relatively rapid shift back to face‐to‐face among child services when in‐person services resumed in May and June 2020. Results further highlight significant differences between child age and service type, with psychiatry less affected by TH than psychotherapy.
Conclusions
Implicit in the data is the ability to offer remotely, a high volume of ongoing behavioral intervention. Findings support TH as less preferred for children than adults while indicating that child TH is favored for psychiatry and support services, less so for psychotherapy. Implications for enhancing child TH delivery and directions for continued research include relational factors, platform (phone/video) and screen salience.
HIGHLIGHTS
Rapid shift to telehealth was successful in maintaining a high volume of mental health services for both adult and children outpatient services despite pandemic.
Significant differences exist between children and adults in the use of telemental healthcare as demonstrated in a robust data record of service utilization.
Service type matters in telemental health with difficulty demonstrated in child psychotherapy, but not in child psychiatry and support services.
Psychotherapy for children via telehealth must be enhanced to optimize impact; salience, attention and fatigue, may be important factors to be addressed for successful implementation.
The COVID‐19 pandemic and the societal response to disease management have led to many significant changes within the healthcare industry (1, 2). Along with the entire healthcare landscape, mental healthcare has experienced a significant shift: in priorities, in population needs and in method of service delivery (1, 3).
One of the most significant changes in mental healthcare has been the rapid shift from in‐person, face‐to‐face (FTF) services to remote, or “telehealth” (TH) services delivered either via video conference or telephone (3, 4). TH per se is not without precedent in mental healthcare (5, 6, 7). Pre‐COVID‐19 research and practice includes strong support for the potential role of TH in mental healthcare (6, 7, 8). However, the recent necessity of rapidly shifting the entire industry from overwhelmingly FTF services to nearly exclusive TH is truly unprecedented and has vastly changed the pace and scale of TH integration (3, 4). Temporarily, TH has been enshrined in law as well, while permanent allowances for TH in medical and mental health services are actively being considered (9).
With this rapid shift and the explosive growth in TH usage, there is relatively little published research that considers children and COVID‐19/TH, though important contributions are beginning to be made (10, 11). Children are undoubtedly a unique population in mental healthcare and not just “little adult patients” (12). It is therefore necessary to assess the use of TH (particularly, tele‐mental health) specifically in a child population. Understanding feasibility, effectiveness, and unique aspects of both provider and client experience is essential to assessing the role and optimizing the use of TH for child mental health.
As described elsewhere (Schechter et al., under review) the current authors (as part of a broader clinical research team at Achieve Behavioral Health [Achieve]) engaged in repeated outreach to both clinical staff and clients to gauge the perceived effectiveness and unique realities of mental health treatment during COVID‐19 lockdown, particularly, the shift to TH services. Similarly, a series of provider surveys were also sent to internal clinical staff and clinicians in other organizations and private practices to understand issues and challenges with TH (see Schechter et al., under review). Data collected from providers indicated a number of areas of perceived difference between TH and standard service delivery including, client interest, provider comfort, service type (psychopharmacology vs. talk therapy), and session focus (see Hoffnung et al., under review).
An important finding of the provider surveys was the consistent report of staff that child services were not identical to adult services, and more specifically, that TH may be less preferred as a method of service delivery for child clients. As one responder in the provider survey from mid‐Corona lockdown aptly summarized: “telehealth is great with adults, good with teens, and a struggle with kids.”
The current study sought to understand possible differences between adults and children in the experience and effectiveness of TH by analyzing the clinic records for the early period of COVID‐19/TH as experienced in New York State.
METHODS
Achieve Behavioral Health
The current study reports on internal review and research conducted at Achieve Behavioral Health (Achieve), a federally designated Certified Community Behavioral Health Center which delivers a broad spectrum of outpatient mental health services to the communities of Rockland and Orange Counties in NY. Achieve employs more than 130 clinical staff members in providing services to over 3200 clients annually. Clinic demographics reflect the clinic catchment area and are heavily influenced by the historically underserved Orthodox Jewish and Hasidic populations which make up a majority of the client population. Demographics for the current sample are listed in Table 1.
| Total sample (N=2520) | ||||
|---|---|---|---|---|
| Age (child/adult) | ||||
| Adult | 44.8% | |||
| Child | 55.2% | |||
| Age (category) | ||||
| 0–6 | 1.9% | |||
| 7–11 | 28.4% | |||
| 12–17 | 24.9% | |||
| 18–64 | 43.4% | |||
| >65 | 1.4% | |||
| Gender (% male) | 56.3% | |||
| Ethnicity | ||||
| White | 96.5% | |||
| Black/African American | 0.7% | |||
| Latino or Hispanic | 1.7% | |||
| Asian American | 0.5% | |||
| Other | 0.6% | |||
| Sessions | Adults (n=1115) | Children (n=1374) | ||
| 21,131 | 22,163 | |||
| N | % | N | % | |
| Date | ||||
| Pre‐lockdown (January 1, 2020 to March 16, 2020) | 8528 | 40.4% | 9830 | 44.4% |
| Lockdown (March 17, 2020 to May 23, 2020) | 7416 | 35.1% | 7322 | 33.0% |
| Post‐lockdown (May 24, 2020 to June 30, 2020) | 5187 | 24.5% | 5011 | 22.6% |
| TH | ||||
| Face‐to‐face | 9789 | 47.0% | 11,948 | 54.3% |
| Telehealth | 11,034 | 53.0% | 10,061 | 45.7% |
| Service | ||||
| Psychotherapy | 12,677 | 60.7% | 14,800 | 67.3% |
| Psychiatry | 2265 | 10.8% | 582 | 2.6% |
| Support services | 3115 | 14.9% | 4093 | 18.6% |
| Other services | 2820 | 13.5% | 2529 | 11.5% |
Participants ‐ Sessions Data
Data represent the total number of sessions of all clinical services rendered across multiple programs (standard outpatient, intensive outpatient, schools, medication management, etc.) as well as multiple departments and service types (psychotherapy, psychiatry, case management, etc.). The data were obtained from the naturally accruing clinical database generated by regular sessions entered in the electronic health records (EHRs).
Total number of sessions included in the analyzed data set is N=43,294, representing 2520 individual clients. All sessions occurred between the dates of January 1, 2020 and June 30, 2020, before, during, and after the peak of COVID‐19 spread in the NY catchment area (see Figure 1 for the number of positive tests in New York State by date).
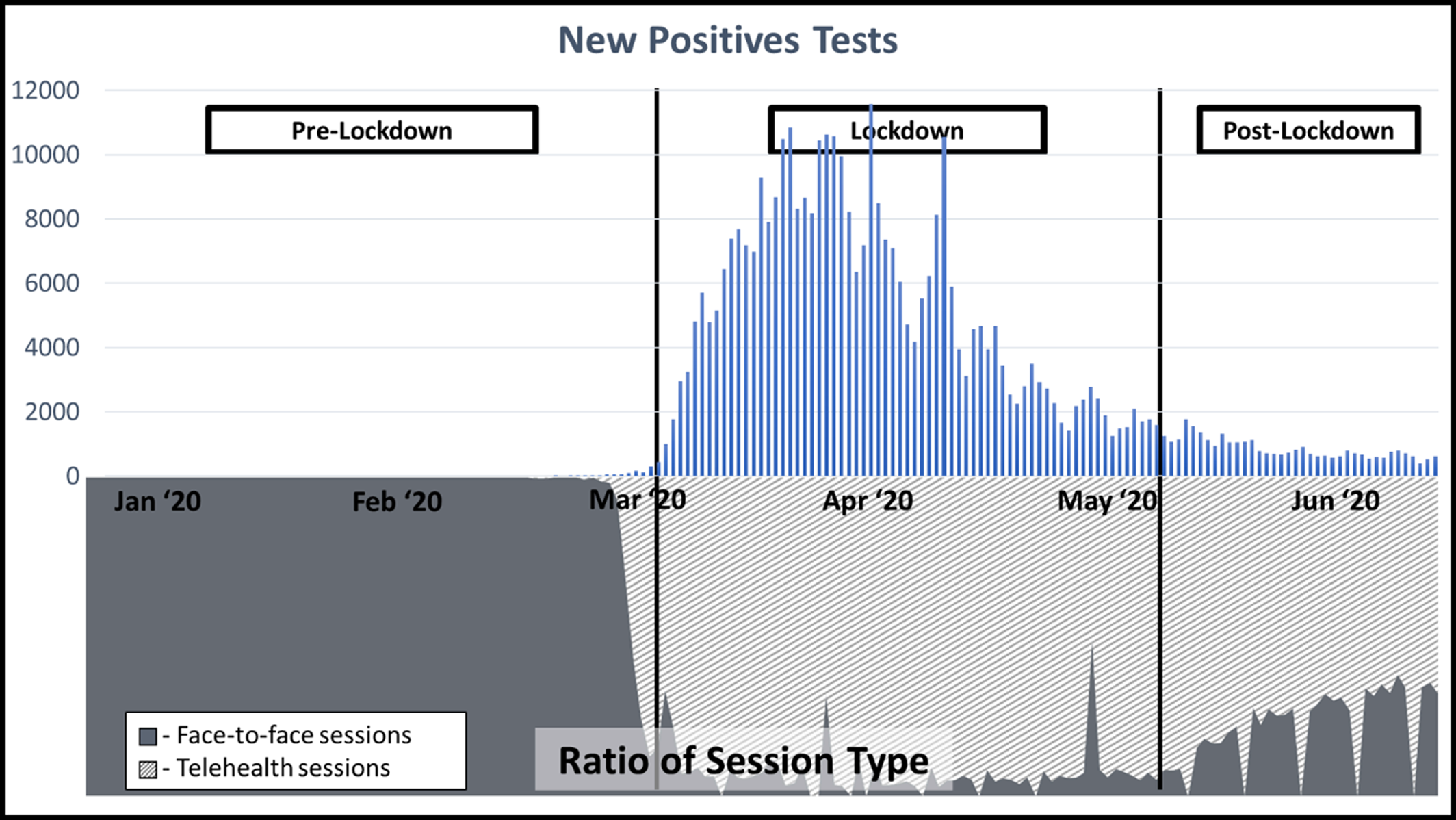
FIGURE 1. Number of positive tests in New York state by date and lockdown period presented above telehealth session type.
In addition, two additional sources of data were used in some analyses, namely record of new calls‐in for service (N=729 recorded for this 6‐month period) and record of discharges (N=575). These records are recorded independently of clinic EHR but represent similar naturally accruing data collected over the course of regular clinic operations.
Data were captured and collated by the Achieve clinical data team and submitted to the research team as anonymized data. No additional data were collected for this study above and beyond that which are collected as part of regular clinic operations. Research was considered exempt from full review. A letter of exemption was received from the Western Copernicus Group Institutional Review Board.
COVID‐19 Context
Data reflect COVID‐19 as experienced in New York State during the first six months of 2020. The COVID‐19 lockdown began over the days of March 15–18, 2020, though, not formalized legally until the following week. The TH executive order in NYS was started retroactively to March 7, 2020. Lockdown restrictions began to be lifted during the week of May 15, 2020 (13). Although Achieve as an “essential service” was never fully closed to in‐person services, with minimal exception, all services were rendered remotely via TH from approximately March 17, 2020 through May 23, 2020. In line with falling infection rates, easing restrictions, and the desire of some clients and providers to resume in‐person services, a slow but steady return to FTF services began beginning May 24, 2020 and continued through the summer.
Hypotheses and Analyses
All analyses were performed using IBM SPSS (version 27). A variety of analytic approaches were necessary given the multiple lines of evidence encompassed in this study as well as the differing natures of data involved. For clarity, the following section is divided by hypothesis and specification of analytic technique is included after each hypothesis.
Use of TH Services: Child Versus Adult
Child serviceswill demonstrate a relative drop when services are delivered via TH as compared to adult services.
It was anticipated that during the period of COVID‐19 necessitated TH (January 1, 2020 to June 30, 2020) total clinical activity would demonstrate a relative drop in child clinical activity when compared to adult clinical activity. As it was further hypothesized that TH would be strongly implicated in this decrease and as TH was not evenly distributed over time, it was necessary to consider, separately and together, the main effects of date, TH and child status (child) on total sessions as well as the interaction of Date×TH×Child. For purposes of analysis, date was stratified across three levels of the COVID‐19 timeline (“1” – pre‐lockdown [January 1, 2020 to March 16, 2020]; “2” – lockdown [March 17, 2020 to May 23, 2020]; “3” – post‐lockdown [May 24, 2020 to June 30, 2020]). An outcome measure of number of sessions was then calculated as a count for each of these three periods with counts stratified by TH (“1” – face‐to‐face; “2” – telehealth). Due to the uneven time periods and the variable presence of individual subjects throughout the duration of the analysis period, an exposure variable (i.e., number of days eligible for sessions) was included as an offset in the analyses. A negative binomial regression analysis was run on count data (number of sessions) using a generalized estimating equation approach to handle repeated measures. Negative binomial regression was indicated over Poisson regression as mean of the outcome (3.11) was substantially smaller than its variance (37.54), indicating overdispersion. Due to the complexity of the above analysis and the inclusion of the three‐way interaction of Date×TH×Child alone includes 12 levels, effects shown to be significant are further reported in the form of descriptive differences.
Significant differences will be demonstrated between different age groups with younger children demonstrating greater drops in services via TH, as compared to older children.
It was further hypothesized that the differences between child and adult sessions would not be uniform across child age, but would indicate fewer sessions for younger children as compared to older children (for this analysis, child clients were divided into three age categories [ages 0–6; 7–11; 12–17 years] consistent with the clinical practice at Achieve). However, it was hypothesized that while different child age groups would be shown to be distinct from one another, it was also anticipated that each group would independently differ from the adult group, thereby lending conceptual validity to the child versus adult structure of analysis. The negative binomial regression was rerun with child replaced by age categories.
Initiation and Retention: Who Stayed in Treatment?
Child clients will show diminished treatment initiation and retention, as demonstrated by diminishing rates of request for new services and increasing rates of discharge when compared to adults over the same time period.
It was expected that records of intake and discharge would display a relative decrease in new requests for services (“calls‐in”) and a relative increase of discharges from service among child clients as compared to adult clients during the study time period. Chi‐square tests of independence were run to measure significance.
Telehealth and Service Type: Psychotherapy, Psychiatry, and Support Services
Data will demonstrate moderating factors in the effect of telehealth on child services, such as differences in services type (e.g., psychiatry vs. psychotherapy)
It was anticipated that while child sessions show a preference for FTF services this preference would not be consistent across service types. In particular, it was expected that psychotherapy sessions would yield a significant preference for FTF over TH, but that this preference would not be observed for child psychiatry sessions. Other categories of services might also display differences, so the factor of service type (“service”) was added to the analyses. In this variable, all sessions are stratified into one of four categories (“1 – psychotherapy; 2 – psychiatry; 3 – support services; 4 – other”). The category of “support services” includes the mental health services of psychiatric rehabilitation, targeted case management and peer support. The category of “other” includes group psychotherapy, crisis, intake, and nursing. Negative binomial regression analysis was repeated including the additional factor of service.
RESULTS
Use of TH Services: Child Versus Adult
Running a fully saturated model that included the main effects of date, TH, and child as well as all interaction terms, it was found that all effects were significant in predicting number of sessions (see Table 2). Despite a greater number of child sessions as compared to adult sessions during the pre‐COVID‐19 period (see Figure 2), total sessions dropped to favor adults during the lockdown period as well as in the post‐lockdown period (see Figure 2). This preference was particularly apparent in TH versus FTF sessions, with adult clients demonstrating an overall preference for TH, exemplified in the significant shift away from TH and return to FTF post‐lockdown, which occurred at twice the rate in child sessions as adult sessions (see Figure 2). Refer Table 1 and Figure 3 for additional representation of the adult preference for TH.
| 95% CI for exp(β) | |||||
|---|---|---|---|---|---|
| Variable | Β | SE | exp(β) | Lower bound | Upper bound |
| Intercept | −2.09 *** | 0.03 | 0.12 | 0.11 | 0.13 |
| Datea | |||||
| Lockdown | −1.84 *** | 0.07 | 0.16 | 0.14 | 0.18 |
| Post‐lockdown | −2.62 *** | 0.07 | 0.07 | 0.06 | 0.08 |
| THb | −4.68 *** | 0.12 | 0.01 | 0.00 | 0.01 |
| Childc | −0.04 | 0.04 | 0.96 | 0.88 | 1.04 |
| Date×THd | |||||
| Lockdown×telehealth | 7.13 *** | 0.13 | 1251.07 | 973.67 | 1607.49 |
| Post‐lockdown×telehealth | 6.38 *** | 0.13 | 589.55 | 457.06 | 760.44 |
| Date×childe | |||||
| Lockdown×child | 0.56 *** | 0.08 | 1.82 | 1.54 | 2.14 |
| Post‐lockdown×child | −0.37 *** | 0.09 | 0.70 | 0.59 | 0.84 |
| TH×childf | −0.83 *** | 0.21 | 0.44 | 0.29 | 0.65 |
| Date×TH×childg | |||||
| Lockdown×telehealth×child | 1.00 *** | 0.22 | 2.71 | 1.77 | 4.16 |
| Post‐lockdown×telehealth×child | −0.22 | 0.21 | 0.81 | 0.53 | 1.23 |
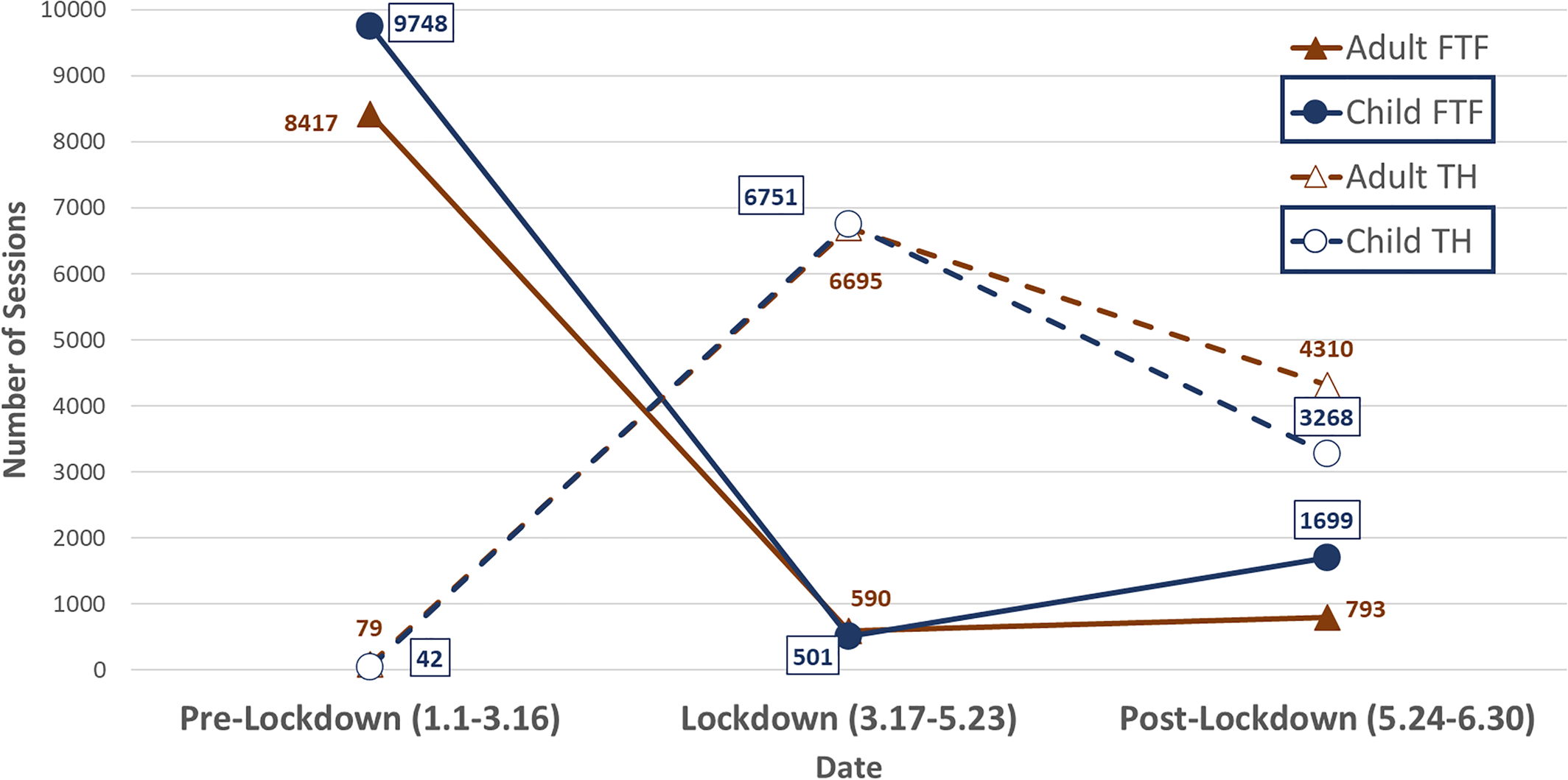
FIGURE 2. Primary study model: Date×TH×Child (outcome: count of sessions), N=43,294.
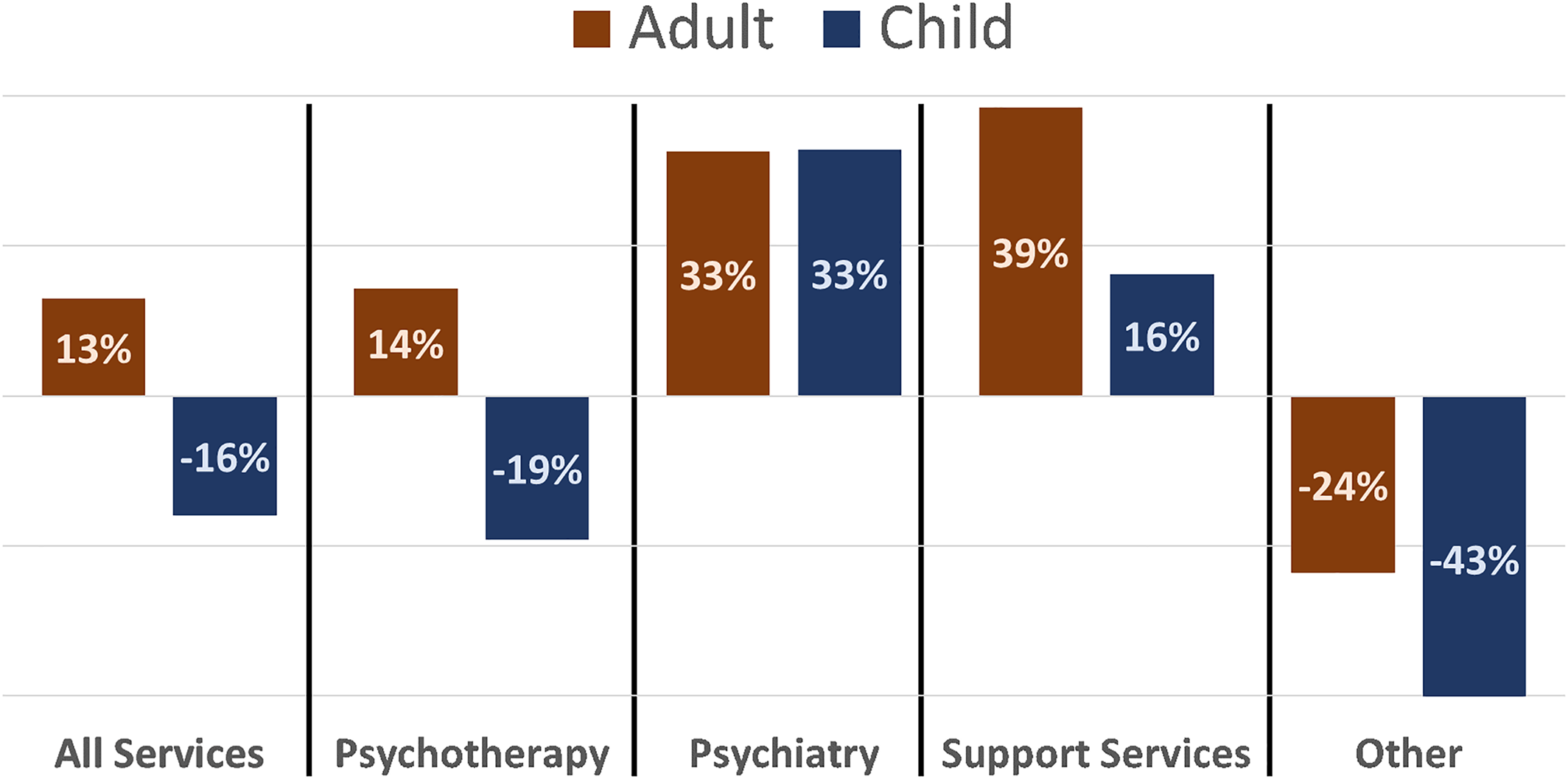
FIGURE 3. Relative change (%) of telehealth services as compared to face‐to‐face services across the entire study period (January 1, 2020–June 30, 2020) stratified by service type and presented by adult and child sessions (n=42,389).
When child status was replaced with the age‐stratification variable, the model and all effects remained significant. Notably, while the interaction of Date×TH×age was significant, consistent with the study hypotheses, the simple effects of age demonstrated significance at every level, with all three child ages demonstrating significant differences when compared to the adult group (“0–6:” χ2(1)=8.879, p=0.003; “7–11:” χ2(1)=6.631, p=0.01; “12–17:” χ2(1)=16.392.88, p<0.001). The model was rerun excluding adult sessions, and child age groups were compared against the reference group of 12–17. In this model, age was significant (Wald χ2(2)=2.542, p=0.02); however, parameter estimates of individual age groups were not significant (0–6: χ2(1)=2.542, p=0.11; 7–11: χ2(1)=3.700, p=0.054).
Initiation and retention: who stayed in treatment?
Monthly records of new calls‐in for service show a significant decline in the number of calls‐in for March and April (corresponding to the COVID‐19 lockdown and switch to TH) as compared to January and February (see Figure 4). New calls‐in began to increase again during May and June. Although the decline was seen in calls‐in for both child and adult clients, the drop in child calls‐in was greater with 114 and 106 calls‐in recorded in January and February falling to 46 and 20 in March and April as compared to adults (January, 78; February, 44; March, 36; April, 22). Furthermore, the increase in calls‐in during the post‐lockdown period was less for child clients relative to their pre‐lockdown numbers (May, 49; June, 80), as compared to adults (May, 61; June, 73). Overall, this difference was found to be significant (χ2(5,N=729) = 21.745, p<0.01).
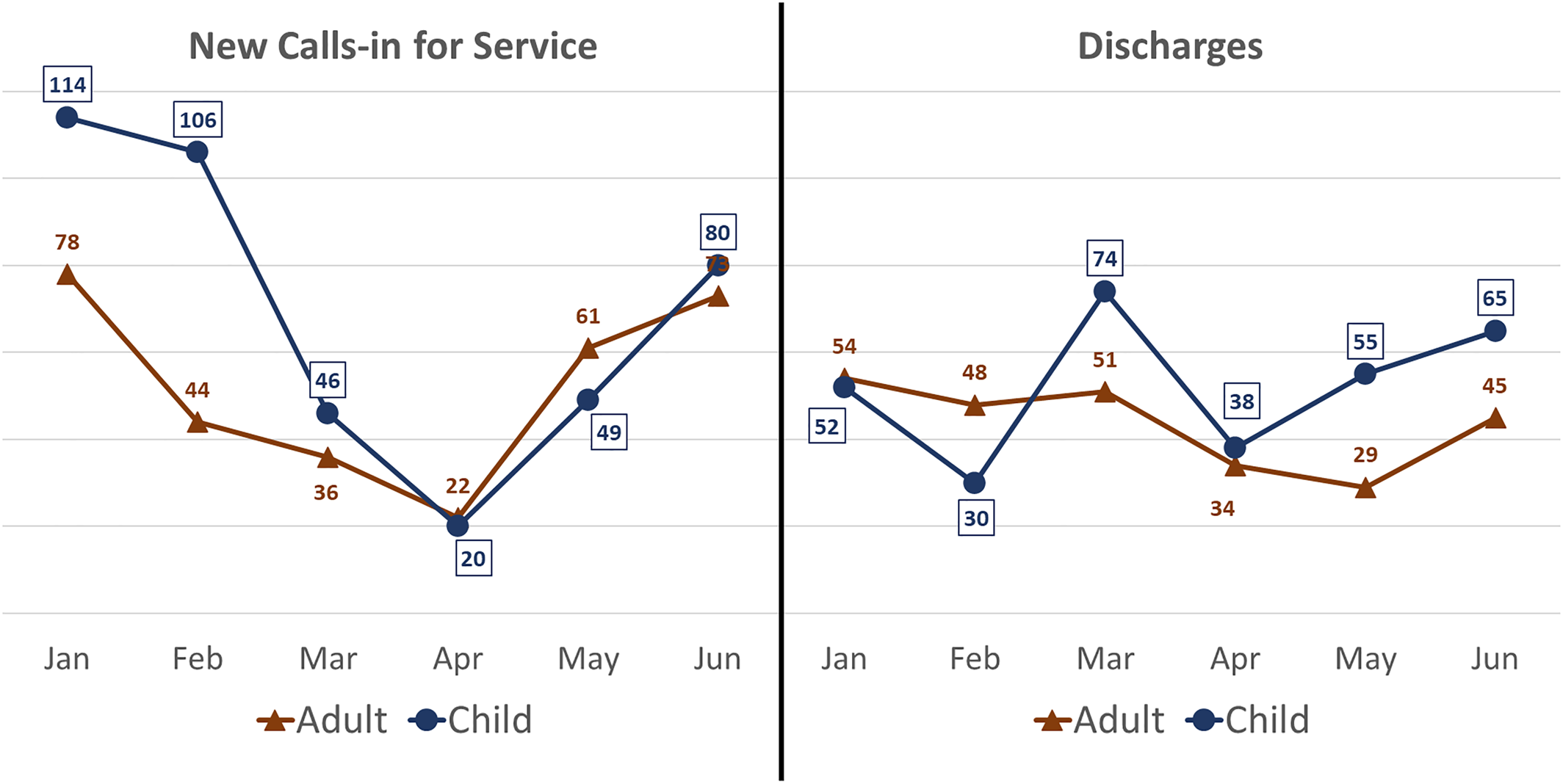
FIGURE 4. Representation of new calls‐in for service (child and adult) as compared with discharges over the six months of the study period (January to June 2020).
Monthly records of discharge from service show a similar, though directionally opposite pattern (see Figure 4). Significant increase in the number of discharges was recorded for the month of March (125) (compared to January [106] and February [78]). Though this increase leveled off in April (72) and May (84) increasing again in June (110), it is noteworthy that the initial increase reflected a significant number of discharges of child clients (March [74] compared to January [52] and February [30]). By contrast adult discharges were steady in March (51, as compared to January [54] and February [48]). This pattern of higher rates of discharge among child clients continued with April (38), May (55) and June (65) as compared to adults (April [34]; May [29]; June [45]). Overall, this difference was found to be significant (χ2(5,N=575)=15.577, p<0.01).
Telehealth and service type: psychotherapy, psychiatry and support services
The original model with Date×TH×Child was rerun with the inclusion of the variable service, and all main and interaction effects were shown to be significant (p<0.05) in predicting number of sessions, including the four‐way interaction Date×TH×Child×service.
As in the previous analysis, the general model of all TH services displayed significant relative decline among child TH services when compared to adult TH services (see Figure 3, as well as Figure 2 and Tables 1 and 2). Child TH services accounted for 16% fewer sessions than did child FTF, compared to adult sessions which showed a 13% increase in TH over FTF sessions. However, as hypothesized, this effect was not uniform across service type. Among psychotherapy sessions, a similar breakdown was demonstrated (child TH: −19%; adult TH: 14%). By contrast, psychiatry sessions increased with TH services and this increase was consistent among child and adult sessions (both demonstrating a 33% increase in TH psychiatry over FTF). Support services sessions also increased across both groups, though more so among adults (39% increase compared to 16% for child sessions). Other services demonstrated significant decline among both child and adult sessions, though here too the decrease was more pronounced among child sessions (adult: −24%; child: −43%).
DISCUSSION
First and foremost, implicit in the data is the ability to offer remotely a high volume of ongoing behavioral interventions, despite physical shutdown and limitations. It is critical to highlight that the behavioral healthcare community can provide uninterrupted access to services and care during turbulent times, despite any concomitant challenges.
In this first large‐scale study of the impact of COVID‐19 on service provision and children, we studied pre, during and post‐COVID switch to TH in a dataset of over 40,000 sessions. We found that there were significant differences between child and adult utilization of TH versus FTF.
TH, as a Service Delivery Method, is Less Preferred for Children Than Adults
Despite comprising a majority of both clients and billed sessions pre‐COVID‐19, children dropped to rates below those of adults with the advent of TH. The co‐occurring decrease in new calls‐in for service and increase in discharge during this same period together with rapid return to FTF services among child sessions not seen among adult sessions further illustrates a preference for FTF services among child clients and providers.
For Children, TH is More Acceptable for Psychiatry and Support Services Than for Psychotherapy
Differences in service type were notable when psychotherapy was compared with psychiatry sessions: whereas number of child psychotherapy sessions decreases significantly when delivered via TH, psychiatry does not, and even increases. A similar pattern holds true for support services. These more pragmatic services may be more useful at these times, but even more importantly, it supports the feasibility of increased access to child psychiatry, a crisis level issue well before the onset of COVID‐19 (14, 15).
Implications
In aggregate, these findings demonstrate the utility of TH broadly, but with potential limits of using TH for children as the mainstay in both general and mental health. The relevance of service type and the significant differences observed among age groups support an even more nuanced approach to evaluation.
In considering the implications of the study results, particularly with areas of future research, it is important to highlight the following possible explanations of the findings.
It may be more difficult to engage a child client in psychotherapy via TH as psychotherapy, in contrast to psychiatry and support services, relies on relationship and communication as critical elements to the intervention itself.
Cognitive fatigue (16) and poor salience in screen‐based communication are likely to be factors which could limit the effectiveness of TH. Both factors are of increased concern among children.
While not immediately linked, there is likely a relationship between child psychotherapy via TH and screen use in the educational system. The ubiquity of screens in the clinical and educational life of the child and young adult (and adult as well!) must be considered, and there may be mutual innovations available from each of these disciplines. The continued development of enhancements to standard practice of remote, screen‐based communications in all sectors is likely to parallel developments in psychotherapy. Simple interventions such as timing, breaks (for physical activity or off‐screen time), joint activity and the like are important areas for research. Reports from providers at Achieve consistently pointed to elements of saliency, engagement, and collaboration as critical to the effectiveness of TH communication with child clients. Evolution of technique is a constant in the field of psychotherapy, continued adaption is required in this new medium.
Overall, it is important to consider this objective report within the context of subjective experience for both clients and providers. As part of a quality assurance response to the COVID‐19 crisis, our staff reached out to N = 65 client families in the months of April and June 2020 to solicit feedback on services. On a scale of 1‐5, 85% of parents felt that the sessions were either helpful (4) or very helpful (5). When asked regarding the quality of services, families were quick to say that while many of their children were struggling with fear and anxiety regarding the COVID‐19 pandemic, their children were receiving strong education about coping skills to reduce anxiety, assistance in scheduling a daily routine and structure, and skills to manage conflict with siblings and parents.
Parents felt that our services have helped both them and their children navigate this extremely difficult time. The ease and consistency of services even led a few respondents to ask whether telehealth could continue even after a potential return to a normal routine. Clearly, the need for service and the relative adequacy of TH lead client parents to value highly this service.
It is telling that our providers were less enthusiastic about TH and child services. As mentioned above, we surveyed providers in April and June 2020 and results consistently pointed to experienced discomfort and perceived inadequacy of child TH services. It will be imperative to consider the interaction of provider and client experience in future research.
Limitations
Data for this study are necessarily focused on service delivery and the association that can be inferred between diminished utilization of services and diminished effectiveness of delivery. While this approach offers a strong general portrayal of TH services, it cannot capture the direct causes of observed changes. Similarly, this analysis cannot determine whether reduction in services is due to client or provider difficulties. While both are essential elements (i.e., clients must find receipt of services comfortable and effective and providers must also find the delivery to be comfortable and effective), the ability to distinguish the cause of any TH treatment difficulty is imperative to focusing efforts at improving the service moving forward. Furthermore, when evaluating child healthcare, the parent or collaterals introduces a third element, not accessible in this dataset, which can be affected by changes in service delivery.
In addition, the study's focus on service utilization and delivery does not necessarily determine treatment effectiveness. The assumption is that psychotherapy and other mental health services are essentially unchanged in content when delivered via TH and it is simply the mode of delivery that differs. Assessing the relative effectiveness of TH versus FTF should be the subject of further research, especially in the area of psychotherapy where treatment and delivery are particularly interdependent.
Also, of importance is the lack of diversity within the study sample. The current report is of culturally unique community. Although culture is a constant within the study, as both adult and child groups compared represent the same cultural context, the likelihood of cultural mediation remains substantial.
Recommendations
The current study represents the first major report on the topic of children and TH. We are continuing to study the many details inherent in this issue and encourage others to do the same. Questions such as outcome versus preference and the relationship of the two, previous relationship versus new online connection (i.e., those with initial sessions FTF who subsequently switch to TH vs. starting with TH), phone versus video, the role of crossover effects (increasing TH screen time concurrent with education and Zoom schooling), as well as establishing specific techniques that optimize child sessions and outcomes. Focused study on the above topics would significantly advance understanding of children in TH.
1
2
3
4
5
6
7
8
9 CMS.gov: Trump administration proposes to expand telehealth benefits permanently for Medicare beneficiaries beyond the COVID‐19 public health emergency and advances access to care in rural areas. [Press release]. https://www.cms.gov/newsroom/press-releases/trump-administration-proposes-expand-telehealth-benefits-permanently-medicare-beneficiaries-beyond. Accessed 3 Aug 2020.Google Scholar
10
11
12
13
14
15
16