Improving the Management of Maternal Mental Health with Digital Health Care
Abstract
Objectives
Digital health solutions have the potential to improve maternal mental health care. The objective of this study is to determine if utilization of a digital health platform, Maven, is associated with improved management of mental health among peripartum people with a history of mental health disorders and determine which components of utilization associate with maternal mental health outcomes.
Methods
Participants in this retrospective cohort analysis (n = 1561) accessed Maven as an employer‐sponsored health benefit and enrolled during their pregnancy and delivered from January 2020 through September 2022. Participants completed health surveys at enrollment, including history of a mood disorder, and post‐delivery. Maven includes online articles, asynchronous and synchronous virtual classes, app‐based mental health screenings, access to allied health professional and maternity care providers via messaging and telehealth appointments. Quantile g–computation was used to estimate the effects of multi‐utilization exposures on reports of postpartum depression (PPD) and management of mental health.
Results
Multi‐utilization exposure mixture models demonstrated that increasing use of digital resources by one quartile is associated with an increased odds of reporting that Maven helped users manage their mental health (aOR: 12.58 [95% CI: 6.74, 23.48]) and was not associated with self‐reported incidence of PPD (aOR: 1.30 [95% CI: 0.52, 3.27]). Care advocate appointments, provider messages, and article reads were positively associated with improved mental health management.
Conclusions
Digital health platforms, such as Maven, may play an important role in managing maternal mental health conditions among pregnant and postpartum people at high risk for PPD.
Highlights
Quantile g–computation was used to estimate the effects of multi‐utilization exposures to a digital health platform, Maven on reports of postpartum depression (PPD) and management of mental health among peripartum people with a history of mental health disorders.
Multi‐utilization exposure mixture models demonstrated that increasing use of digital resources by one quartile is associated with an increased odds of reporting that Maven helped users manage their mental health and was not associated with self‐reported incidence of PPD.
Digital health platforms, such as Maven, may play an important role in managing maternal mental health conditions among pregnant and postpartum people at high risk for PPD.
Maternal mental health conditions are the leading cause of maternal mortality, primarily due to suicide and drug overdose, and account for 22.7% of all maternal deaths in the United States (1, 2). Postpartum depression (PPD), a common maternal mental health condition, affects 16%–25% of peripartum people and carries significant maternal and child morbidity (3). In addition to maternal suffering, maternal depression increases the risk for suicide, substance use, premature birth, and low birthweight (4) and has significant consequences for children's development including an increased risk of cognitive, behavioral, and mental health problems (5, 6).
The significant maternal and child morbidity and maternal mortality associated with PPD is largely preventable. Analysis provided by Maternal Morbidity and Mortality Review Committees from 14 states reported that 100% of maternal mental health related deaths reviewed were preventable by improving screening, assessment, and referral and access to effective mental health treatments and psychosocial supports as well as improving patient‐provider and provider‐provider communication and care coordination (7, 8). Furthermore, there are well‐established effective interventions that can prevent the onset of new cases of PPD, particularly for those with a history of mental health conditions. In a review of 50 studies evaluating interventions to prevent PPD among high‐risk pregnant or postpartum people, the United States Preventative Services Task Force found convincing evidence to support the use of counseling interventions such as Cognitive Behavioral Therapy and Interpersonal Psychotherapy for the prevention of PPD (9, 10). Recent work has also demonstrated that relatively simple and practical educational interventions are effective at reducing the risk of PPD (11, 12).
Despite strong evidence supporting preventative intervention for those at high risk for PPD and recommendations to screen, assess and refer patients to mental health treatment, current systems of care are not meeting the basic maternal mental health needs of pregnant and postpartum people. Preventative interventions are not available or accessible to most patients due to the lack of highly trained specialists needed to deliver these interventions (13). Only 1 in 5 pregnant and 1 in 8 postpartum people are screened for PPD (14), and <20% of those in need of mental health care will receive treatment (15). The breadth of recommended screenings, and the depth of knowledge needed to adequately assess and appropriately connect peripartum women to treatment and/or needed resources is difficult to obtain in our current health systems (16). Insufficient time, unfamiliarity with screening tools, lack of knowledge about mental health conditions and the limited availability of treatment services, particularly in rural underserved areas (17) are the reasons most cited for not adopting evidence‐based screening and referral practices (18, 19). Individual patient factors such as lack of knowledge about mental health and stigma are potent barriers to treatment (20). Treatment services are often located in a healthcare system outside of where peripartum women receive their obstetric care resulting in a lack of communication and coordination of care between providers. Care is further fragmented across health systems where past screening and treatment information is not available to current providers (20, 21).
Digital health solutions have the potential to create better systems of care for all pregnant and postpartum people at risk for or experiencing maternal mental health conditions (22, 23, 24). Simple app‐based technologies are easily accessible and widely available to peripartum populations and can deliver relevant educational content to increase knowledge and awareness about maternal mental health conditions. Additionally, digital health solutions can provide effective screenings and immediate support from non‐licensed mental health workers to address mental health concerns and other psychosocial needs during the peripartum period (25) as well as improve communication and care coordination between patients and providers (22). Digital health solutions can extend the reach of the limited number of mental health providers and afford greater access to readily available and easily accessible mental health care via telehealth (22, 23, 26).
Maven is a comprehensive women's and family health digital platform that was developed to provide support services that supplement and complement routine prenatal and postpartum care through telehealth services. Users receive free and unlimited access to Maven as an employer‐sponsored health benefit through their own or their partner's employer or through their health insurance provider. Maven affords pregnant and postpartum people access to educational materials via online articles, synchronous and asynchronous virtual classes, app‐based mental health screenings with efficient access to allied health professionals (e.g., social workers, nurses) and maternity care providers via messaging and telehealth appointments. Importantly allied health professionals can provide mental health support, and/or referrals to mental health treatment and assist with care coordination and communication during the peripartum period. Given Maven's comprehensive approach to maternity care, including elements necessary to better identify and treat mental health conditions during pregnancy and the postpartum period, it is possible that this digital health platform can potentially reduce the self‐reported incidence of PPD and support the management of mental health conditions among those at high risk for PPD.
The aims of this study are to examine: (1) if utilization of Maven during pregnancy is associated with a lower self‐reported incidence of PPD and report of improved management of mental health among a high‐risk population (i.e., those with a history of anxiety, depression, perinatal mood disorder, or PPD); (2) which components of virtual care within the maternal health platform, including mental health provider appointments, have the greatest association with the self‐reported incidence of PPD, and on report of management of mental health; and (3) if the report of PPD is associated with the participants' perception that Maven helped users to better manage their mental health.
METHODS
Study Design and Setting
This retrospective cohort analysis assessed the association between user engagement with a digital health platform during pregnancy and user report of PPD and management of mental health among a high‐risk population. Users received access to the digital platform as an employer‐sponsored health benefit through their own or their partner's employer or through their health plan. We included users who enrolled in the program during their pregnancy and delivered from January 2020 through September 2022. Users were included if they completed the onboarding health survey at enrollment, completed the post‐delivery health survey within a year of their infant's birth, reported a history of a mood disorder (i.e., participants selected any of “history of mood disorder, depression, anxiety, or PPD” from a list of medical and mental health conditions), and their zip code could be mapped to the CDC's Social Vulnerability Index (SVI) (Figure 1).
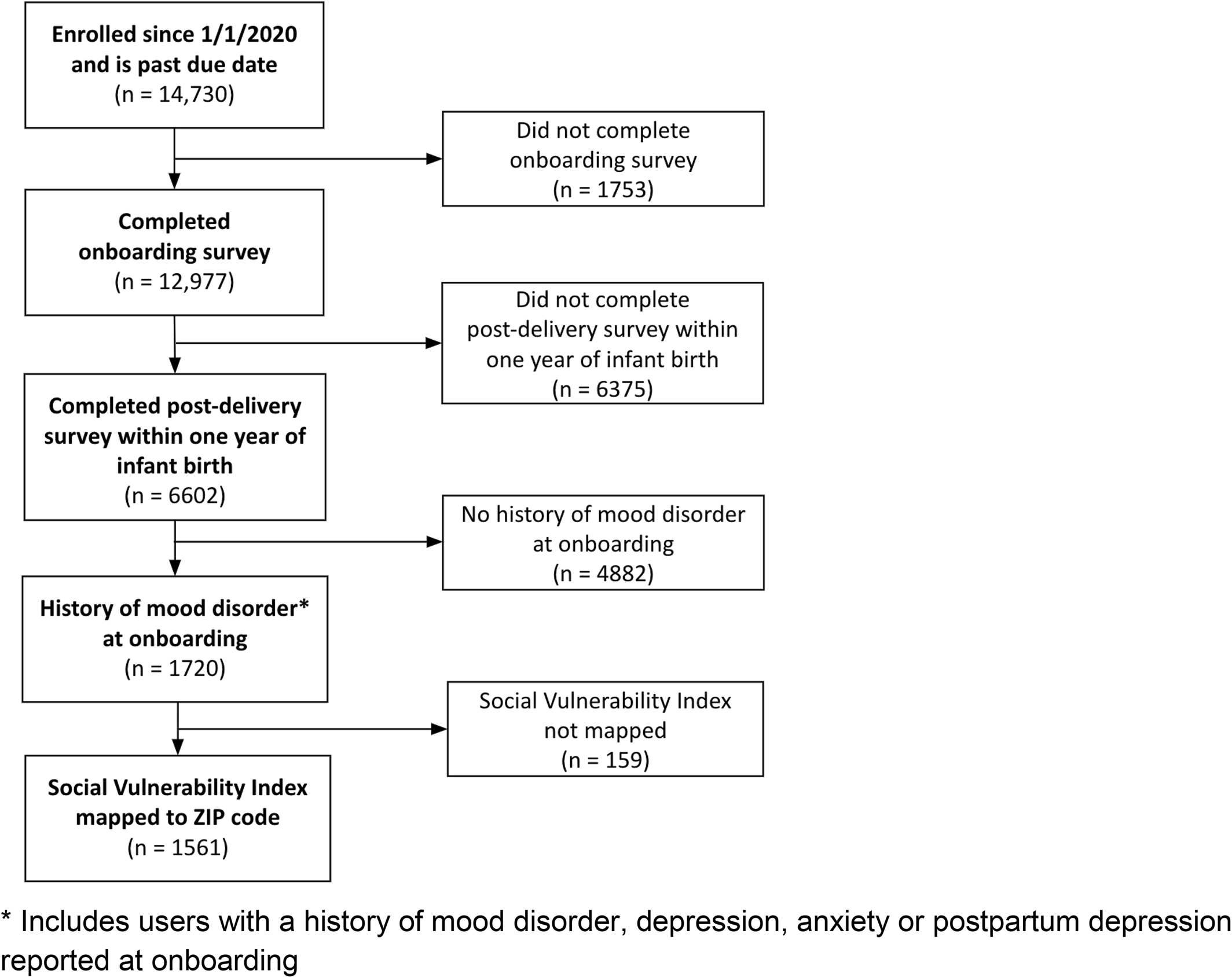
FIGURE 1. Cohort flowchart.
The study protocol was designated as exempt by WCG Institutional Review Board, an independent ethical review board. All users consented to the use of their de‐identified data for scientific research upon creating an account. All data used in this analysis were de‐identified.
Digital Platform Description and Data Collection
Digital resources available on the platform include access to: (1) educational content (articles, class recordings, and live virtual classes), (2) care coordination through a care advocate (CA), and (3) provider services. Educational content: Educational content available included articles, class recordings, and live virtual classes. Articles address a range of themes of interest during pregnancy, as well as mental health‐specific content (e.g., “4 mental exercises to combat pregnancy anxiety” and “Spotting the signs of PPD and anxiety”). Class recordings are available for users to watch at any time, and include content on a variety of topics (e.g., “Childbirth education 101” and “How to manage stress and anxiety”). Live virtual classes are also held, and they provide a forum in which users can engage with a health care provider in a group setting to learn and ask questions. Care coordination: All users are assigned a CA, who is an allied health professional (e.g., nurses, social workers, etc) who serves as a user's primary point of contact within the digital platform. CAs support the coordination of digital prenatal services and direct users to providers and services (both virtual and in‐person when necessary). Users can interact with CAs through messages and virtual appointments. Provider services: Users have access to a variety of healthcare providers on the digital platform, including obstetrician/gynecologists (OB/GYNs), doulas, midwives, mental health providers, nutritionists, wellness coaches, and others. Users can interact with providers through messages and virtual appointments. All utilization of digital resources were tracked within the product.
The key study outcomes, collected in the post‐delivery survey, were (1) whether a user reported PPD and (2) whether a user reported that Maven helped them manage their anxiety and/or depression. To assess these outcomes, users were asked to select “Have you experienced any of the following during this pregnancy?” where users were offered the option to select “postpartum depression” as one of several response options from a list of gestational conditions and “In what way(s) did Maven influence your experience?” where users were offered the option to select “Maven helped me manage anxiety and/or depression” as one of a variety of response options from a list of ways in which Maven may have helped the user.
User demographics and health data were self‐reported. Age at onboarding was calculated internally from the user's date of birth. Race and ethnicity were asked in the same question, and race was categorized into Hispanic/Latinx, and non‐Hispanic/Latinx: White, Asian or Pacific Islander, Black, and Other (which, due to small sample sizes, was composed of multiracial and American Indian users). Medical and mental health conditions were assessed by user self‐report on the onboarding survey. Pregnancy‐related conditions were assessed by user‐self report and were included as present if a user reported them on either the onboarding survey or the post‐delivery survey. We used the CDC's SVI as a proxy for social determinants of health (25). SVI was assigned to each user based on ZIP code (methods described previously 26). SVI was dichotomized into low (≤0.80) and high (>0.80), with high representing the highest‐risk quintile nationally.
Statistical Analysis
Statistical analysis was performed using R v.3.6.3 (27). We used descriptive statistics to assess users' demographics, medical conditions, digital platform utilization during pregnancy, and relevant outcomes, stratified by a report of PPD on the post‐delivery survey. In bivariate analyses, Chi‐square or Fisher's exact test were used to assess categorical variables, and t‐tests and Mann‐Whitney U‐tests were used to assess continuous variables.
Single‐exposure approach
We quantified bivariate associations between utilization exposures using a Spearman correlation matrix (Figure S1). We then used adjusted logistic regression models to estimate the odds ratios and 95% confidence intervals (CI) for each utilization exposure (in quartiles) and both outcomes: PPD and report of help to manage anxiety and/or depression. We used directed acyclic graphs to identify confounders and determine the covariates in each model (28). Models were adjusted for maternal age, race/ethnicity, parity, thyroid disease, SVI, and timing of completing the post‐delivery survey.
Multi‐exposure approach
Since users often use more than one kind of digital resource (e.g., reading articles and attending appointments with providers), in addition to assessing how use of individual types of resources influence outcomes, we were interested in assessing the impact of utilizing a combination of digital resources on our outcomes. We used quantile g–computation to estimate the joint association between mixtures of utilization and PPD. Quantile g‐computation has been described previously (29). Briefly, this method estimates the joint effect of a one quantile increase in the exposure level of simultaneous exposures of a mixture on an outcome. While this method was adapted from weighted quantile sum regression, quantile g‐computation differs in that it does not require directional homogeneity, allowing different components of the mixture to have either negative or positive effects on the outcome (29). This method first categorizes exposures into quartiles that are fitted onto regression models. Each exposure takes on a positive or negative weight, and the weights of all components of the mixture sum to 1. If directional homogeneity does not apply, an individual exposure's weight can be interpreted as the proportion of the positive (or negative) partial effect on the outcome. In this case, positive weights will sum to 1 and negative weights will sum to 1. Here we report the conditional odds ratio and estimate the joint effect of utilization of various digital resources on PPD and management of anxiety and/or depression in both crude and adjusted models. Adjusted models control for the same covariates as single‐exposure models. Quantile g–computation was performed using the “qgcomp” package version 2.10.1.
Logistic regression was used to assess whether a report of PPD is associated with the participants' perception that Maven helped them to better manage their mental health as well as to assess whether having at least one virtual appointment with a mental health provider is associated with PPD.
RESULTS
The study population included 1561 pregnant users of a digital health platform who had a history of a mood disorder reported at onboarding. Full inclusion criteria are shown in Figure 1. User characteristics, including demographics, medical conditions, utilization of digital resources, and relevant user‐reported outcomes are included in Table 1. Users had a mean age of approximately 33 years and most were nulliparous (67.9%). Compared to other categories of body mass index, more users were normal weight (46.3%), and most users were non‐Hispanic, White (53.7%). Users who reported PPD on the post‐delivery survey were more likely to be younger, parous, non‐White, and live in an area with a higher SVI. These users were also more likely to report high blood pressure, thyroid disease, fetal growth restriction, depression, a history of perinatal mood disorder, and a history of PPD. Users with PPD differed from those without PPD in their digital utilization of articles, class recordings, and virtual classes on the platform, and they were more likely to have completed the post‐delivery survey later (p < 0.05).
| Postpartum depression | Overall (n = 1561) | p‐value | ||
|---|---|---|---|---|
| No (n = 1406) | Yes (n = 155) | |||
| Demographics | ||||
| Age (mean [SD]) | 32.8 (4.24) | 31.5 (4.54) | 32.7 (4.28) | <0.001 |
| Parity, n (%) | 0.03 | |||
| Nulliparous | 967 (68.8%) | 93 (60.0%) | 1060 (67.9%) | |
| Parous | 439 (31.2%) | 62 (40.0%) | 501 (32.1%) | |
| Body mass index classification (kg/m2), n (%)b | 0.46 | |||
| Underweight (<18.5) | 33 (2.3%) | 2 (1.3%) | 35 (2.2%) | |
| Normal (18.5 to <25.0) | 653 (46.4%) | 69 (44.5%) | 722 (46.3%) | |
| Overweight (25.0 to <30.0) | 379 (27.0%) | 51 (32.9%) | 430 (27.5%) | |
| Obese (≥30.0) | 303 (21.6%) | 30 (19.4%) | 333 (21.3%) | |
| Race/ethnicity, n (%) | 0.02 | |||
| White | 774 (55.0%) | 65 (41.9%) | 839 (53.7%) | |
| Hispanic | 154 (11.0%) | 27 (17.4%) | 181 (11.6%) | |
| Asian or Pacific Islander | 150 (10.7%) | 18 (11.6%) | 168 (10.8%) | |
| Black | 74 (5.3%) | 8 (5.2%) | 82 (5.3%) | |
| Otherc | 34 (2.4%) | 6 (3.9%) | 40 (2.6%) | |
| I prefer not to say | 220 (15.6%) | 31 (20.0%) | 251 (16.1%) | |
| High social vulnerability index, n (%) | 44 (3.1%) | 12 (7.7%) | 56 (3.6%) | 0.01 |
| Medical conditions, n (%) | ||||
| Chronic conditions | ||||
| Heart disease | 9 (0.6%) | 2 (1.3%) | 11 (0.7%) | 0.30 |
| Diabetes | 13 (0.9%) | 2 (1.3%) | 15 (1.0%) | 0.65 |
| High blood pressure | 94 (6.7%) | 11 (7.1%) | 105 (6.7%) | 0.04 |
| Blood disorder | 17 (1.2%) | 1 (0.6%) | 18 (1.2%) | 0.99 |
| Thrombophilia | 12 (0.9%) | 1 (0.6%) | 13 (0.8%) | 0.99 |
| Kidney disease | 6 (0.4%) | 1 (0.6%) | 7 (0.4%) | 0.52 |
| Thyroid disease | 120 (8.5%) | 14 (9.0%) | 134 (8.6%) | 0.04 |
| Autoimmune disease | 60 (4.3%) | 6 (3.9%) | 66 (4.2%) | 0.05 |
| Pregnancy‐related conditions | ||||
| Cholestasis | 28 (2.0%) | 4 (2.6%) | 32 (2.1%) | 0.55 |
| Fetal growth restriction | 39 (2.8%) | 10 (6.5%) | 49 (3.1%) | 0.02 |
| Gestational hypertension | 258 (18.4%) | 30 (19.4%) | 288 (18.4%) | 0.09 |
| Preeclampsia | 117 (8.3%) | 15 (9.7%) | 132 (8.5%) | 0.54 |
| Gestational diabetes | 165 (11.7%) | 14 (9.0%) | 179 (11.5%) | 0.32 |
| Mental health conditions | ||||
| Depression | 652 (46.4%) | 93 (60.0%) | 745 (47.7%) | 0.001 |
| Anxiety | 1215 (86.4%) | 125 (80.6%) | 1340 (85.8%) | 0.05 |
| Perinatal mood disorder | 38 (2.7%) | 10 (6.5%) | 48 (3.1%) | 0.01 |
| History of postpartum depression | 193 (13.7%) | 42 (27.1%) | 235 (15.1%) | <0.001 |
| Utilization, n (%) | ||||
| Articles readd | ||||
| [0, 7] | 353 (25.1%) | 61 (39.4%) | 414 (26.5%) | <0.001 |
| (7, 20] | 347 (24.7%) | 41 (26.5%) | 388 (24.9%) | |
| (20, 47] | 336 (23.9%) | 34 (21.9%) | 370 (23.7%) | |
| (47, 401] | 370 (26.3%) | 19 (12.3%) | 389 (24.9%) | |
| Class recordings watchedd | ||||
| 0 | 676 (48.1%) | 96 (61.9%) | 772 (49.5%) | 0.01 |
| (0, 1] | 217 (15.4%) | 21 (13.5%) | 238 (15.2%) | |
| (1, 3] | 193 (13.7%) | 16 (10.3%) | 209 (13.4%) | |
| (3, 34] | 320 (22.8%) | 22 (14.2%) | 342 (21.9%) | |
| Virtual classes attendedd | ||||
| 0 | 808 (57.5%) | 105 (67.7%) | 913 (58.5%) | 0.04 |
| (0, 2] | 342 (24.3%) | 26 (16.8%) | 368 (23.6%) | |
| (2, 16] | 256 (18.2%) | 24 (15.5%) | 280 (17.9%) | |
| Appointments with CAd | ||||
| 0 | 476 (33.9%) | 53 (34.2%) | 529 (33.9%) | 0.90 |
| 1 | 825 (58.7%) | 92 (59.4%) | 917 (58.7%) | |
| (1, 9] | 105 (7.5%) | 10 (6.5%) | 115 (7.4%) | |
| Messages sent to CAd | ||||
| 0 | 564 (40.1%) | 67 (43.2%) | 631 (40.4%) | 0.62 |
| (0, 1] | 183 (13.0%) | 19 (12.3%) | 202 (12.9%) | |
| (1, 5] | 316 (22.5%) | 38 (24.5%) | 354 (22.7%) | |
| (5, 76] | 343 (24.4%) | 31 (20.0%) | 374 (24.0%) | |
| Appointments with providersd | ||||
| 0 | 622 (44.2%) | 80 (51.6%) | 702 (45.0%) | 0.37 |
| (0, 1] | 232 (16.5%) | 22 (14.2%) | 254 (16.3%) | |
| (1, 3] | 242 (17.2%) | 22 (14.2%) | 264 (16.9%) | |
| (3, 83] | 310 (22.0%) | 31 (20.0%) | 341 (21.8%) | |
| Messages sent to providersd | ||||
| 0 | 860 (61.2%) | 99 (63.9%) | 959 (61.4%) | 0.68 |
| (0, 2] | 227 (16.1%) | 21 (13.5%) | 248 (15.9%) | |
| (2, 196] | 319 (22.7%) | 35 (22.6%) | 354 (22.7%) | |
| Appointments with mental health providerse | ||||
| 0 | 1182 (84.1%) | 124 (80.0%) | 1306 (83.7%) | 0.19 |
| 1 or more | 224 (15.9%) | 31 (20.0%) | 255 (16.3%) | |
| Days from baby day of birth to completion of the post‐delivery survey (mean [SD]) | 18.5 (33.6) | 44.7 (59.9) | 21.1 (37.9) | <0.001 |
| User‐reported outcomes, n (%) | ||||
| Maven helped me manage anxiety and/or depression | 277 (19.7%) | 38 (24.5%) | 315 (20.2%) | 0.16 |
In single‐digital resource utilization models, adjusted logistic regression showed that reading articles on the platform (quartile 4: aOR: 0.44 [95% CI: 0.24, 0.78]) is significantly associated with lower odds of reporting PPD (Table 2). Adjusted logistic regression also found that reading articles, watching class recordings, attending CA appointments, sending messages to CAs, attending provider appointments, and sending messages to providers on the platform are each significantly associated with higher odds of reporting that the platform helped the user manage anxiety and/or depression (Table 2).
| Utilization | Odds of postpartum depression (95% CI) | Odds of reporting that the platform helped the user manage anxiety and/or depression | ||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | p | Adjustedb | p | Unadjusted | p | Adjustedb | p | |
| Article reads | ||||||||
| 0 | Ref | Ref | Ref | Ref | ||||
| (7, 20] | 0.68 (0.45, 1.04) | 0.078 | 0.81 (0.52, 1.26) | 0.4 | 0.88 (0.61, 1.29) | 0.5 | 0.91 (0.62, 1.34) | 0.6 |
| (20, 47] | 0.59 (0.37, 0.91) | 0.018 | 0.83 (0.51, 1.34) | 0.4 | 1.21 (0.84, 1.73) | 0.3 | 1.26 (0.86, 1.84) | 0.2 |
| (47, 401] | 0.3 (0.17, 0.50) | <0.001 | 0.44 (0.24, 0.78) | 0.006 | 1.9 (1.36, 2.68) | <0.001 | 2.11 (1.46, 3.07) | <0.001 |
| Class recordings | ||||||||
| 0 | Ref | Ref | Ref | Ref | ||||
| (0, 1] | 0.68 (0.41, 1.10) | 0.13 | 0.84 (0.49, 1.39) | 0.5 | 1.46 (1.02, 2.08) | 0.037 | 1.46 (1.01, 2.11) | 0.042 |
| (1, 3] | 0.58 (0.32, 0.99) | 0.056 | 0.82 (0.45, 1.43) | 0.5 | 1.61 (1.11, 2.31) | 0.011 | 1.7 (1.15, 2.48) | 0.007 |
| (3, 34] | 0.48 (0.29, 0.77) | 0.003 | 0.69 (0.41, 1.15) | 0.2 | 1.55 (1.13, 2.11) | 0.006 | 1.67 (1.19, 2.34) | 0.003 |
| Virtual classes | ||||||||
| 0 | Ref | Ref | Ref | Ref | ||||
| (0, 2] | 0.59 (0.37, 0.90) | 0.02 | 0.72 (0.44, 1.13) | 0.2 | 0.92 (0.68, 1.25) | 0.6 | 0.98 (0.71, 1.34) | 0.9 |
| (2, 16] | 0.72 (0.44, 1.13) | 0.2 | 0.98 (0.58, 1.61) | >0.9 | 1.07 (0.77, 1.48) | 0.7 | 1.21 (0.85, 1.73) | 0.3 |
| CA appointments | ||||||||
| 0 | Ref | Ref | Ref | Ref | ||||
| 1 | 1.00 (0.70, 1.44) | >0.9 | 1.26 (0.87, 1.86) | 0.2 | 1.83 (1.35, 2.51) | <0.001 | 1.91 (1.40, 2.64) | <0.001 |
| (1, 9] | 0.86 (0.40, 1.67) | 0.7 | 1.21 (0.55, 2.44) | 0.6 | 11.5 (7.32, 18.3) | <0.001 | 11.7 (7.33, 19.1) | <0.001 |
| CA messages | ||||||||
| 0 | Ref | Ref | Ref | Ref | ||||
| (0, 1] | 0.87 (0.50, 1.47) | 0.6 | 0.97 (0.55, 1.67) | >0.9 | 1.7 (1.10, 2.57) | 0.014 | 1.62 (1.05, 2.47) | 0.03 |
| (1, 5] | 1.01 (0.66, 1.53) | >0.9 | 1.24 (0.79, 1.93) | 0.3 | 2.07 (1.47, 2.92) | <0.001 | 2.04 (1.44, 2.90) | <0.001 |
| (5, 76] | 0.76 (0.48, 1.18) | 0.2 | 1 (0.62, 1.60) | >0.9 | 3.27 (2.37, 4.52) | <0.001 | 3.3 (2.36, 4.62) | <0.001 |
| Provider appointments | ||||||||
| 0 | Ref | Ref | Ref | Ref | ||||
| (0, 1] | 0.74 (0.44, 1.19) | 0.2 | 0.91 (0.53, 1.50) | 0.7 | 1.36 (0.89, 2.06) | 0.15 | 1.33 (0.86, 2.01) | 0.2 |
| (1, 3] | 0.71 (0.42, 1.14) | 0.2 | 0.85 (0.50, 1.40) | 0.5 | 2.72 (1.89, 3.91) | <0.001 | 2.79 (1.93, 4.05) | <0.001 |
| (3, 83] | 0.78 (0.50, 1.19) | 0.3 | 1.06 (0.65, 1.67) | 0.8 | 5.12 (3.72, 7.07) | <0.001 | 5.09 (3.65, 7.15) | <0.001 |
| Provider messages | ||||||||
| 0 | Ref | Ref | Ref | Ref | ||||
| (0, 2] | 0.80 (0.48, 1.29) | 0.4 | 0.97 (0.57, 1.59) | >0.9 | 1.91 (1.35, 2.69) | <0.001 | 1.89 (1.32, 2.68) | <0.001 |
| (2, 196] | 0.95 (0.63, 1.42) | 0.8 | 1.18 (0.76, 1.80) | 0.5 | 3.42 (2.57, 4.55) | <0.001 | 3.39 (2.52, 4.57) | <0.001 |
In both unadjusted and adjusted models, results from the multi‐utilization exposure mixture showed that simultaneously increasing use of all digital resources by one quartile was not associated with report of PPD (aOR: 1.30 [95% CI: 0.52, 3.27]), but it was associated with an increased odds of reporting that Maven helped the user manage their anxiety and/or depression (aOR: 12.58 [95% CI: 6.74, 23.48]) (Figure 2). Quantile g‐computation also demonstrated that within the digital resource utilization mixture, provider messages and virtual classes seemed to drive the positive associations with PPD, while CA appointments, provider appointments, and CA messages were also positively associated with PPD but with smaller weights in adjusted models (Figure 3). Article reads and class recordings had a negative association with PPD in adjusted models, with articles accounting for the largest weight (Figure 3). For improved management of mental health, CA appointments seem to be the biggest driving factor for the positive association with the outcome, with provider appointments, provider messages, and article reads contributing smaller positive weights. Within the mixture, virtual classes, CA messages, and class recordings are negatively associated with reports of improved mental health management.
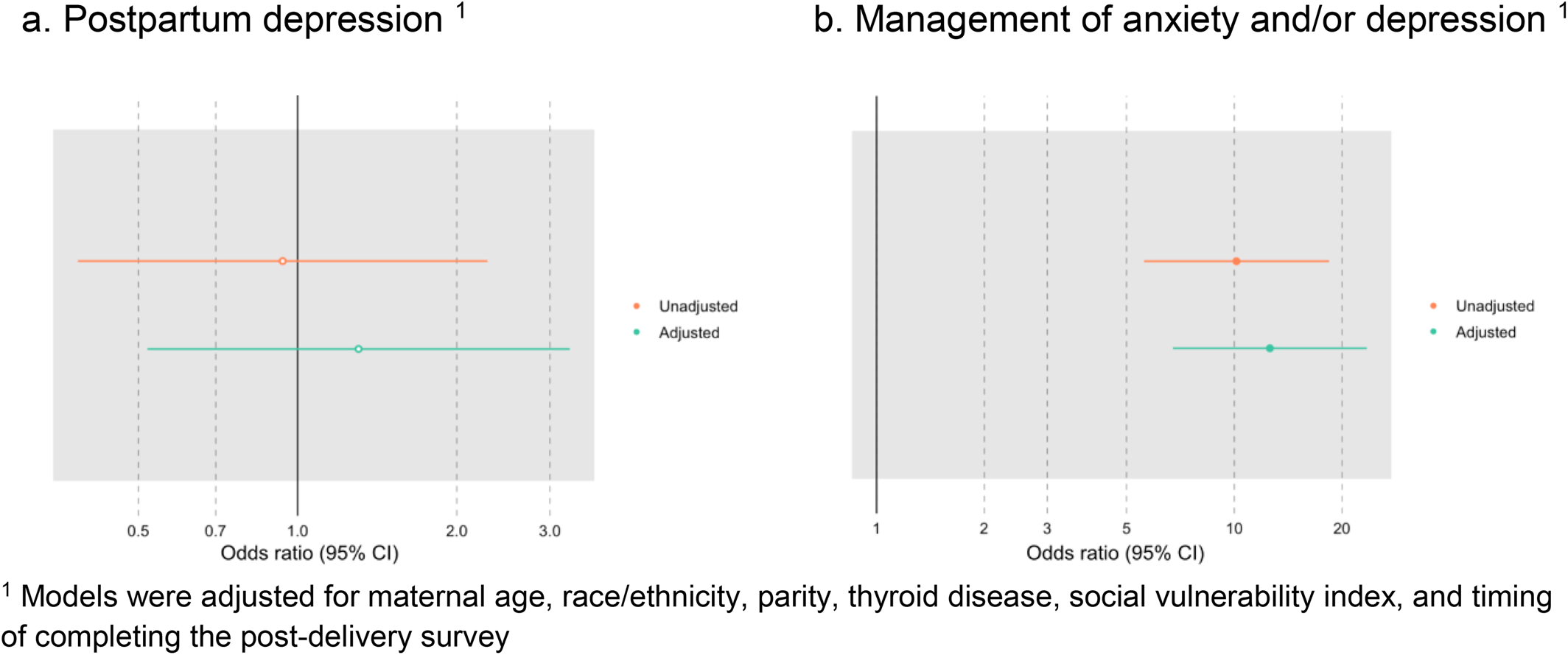
FIGURE 2. Unadjusted and adjusted OR (95% CI) of outcomes associated with a one quartile increase in all digital resource exposures. CI, confidence interval; OR, odds ratios.
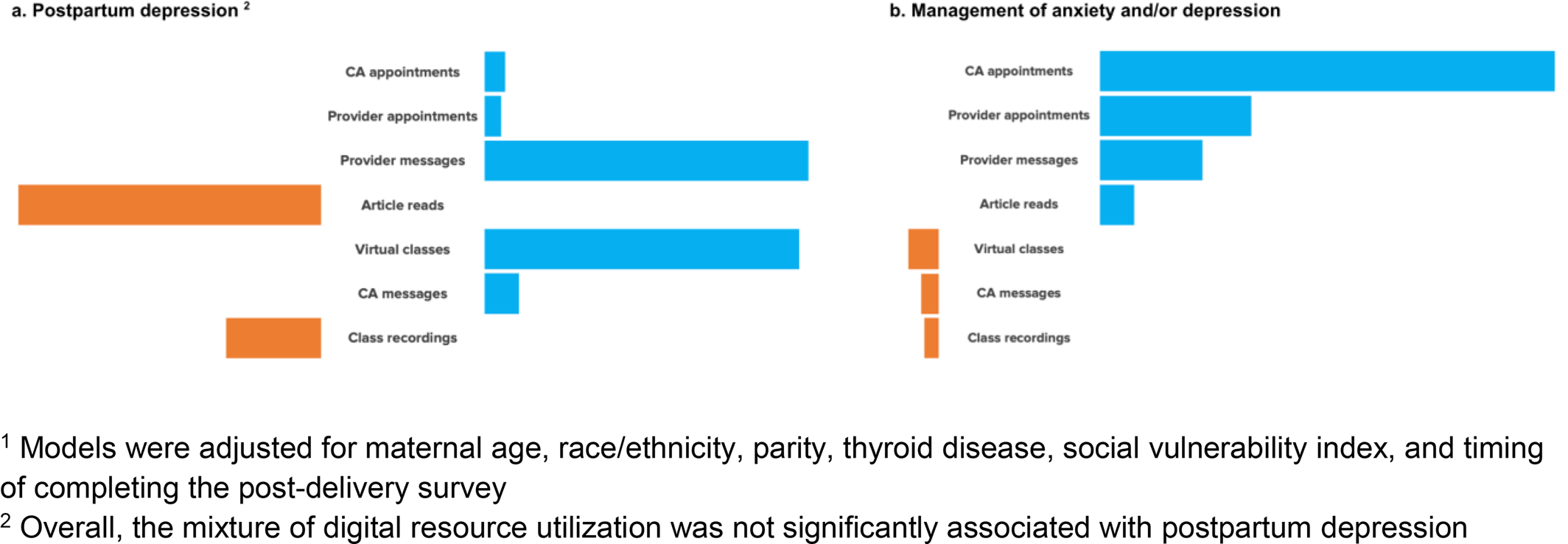
FIGURE 3. Impact of utilization of digital resources as mixtures on postpartum depression and management of anxiety and/or depression (adjusted).1
Report of PPD was positively, but not significantly, associated with a report of the platform helping users to manage anxiety and/or depression (aOR: 1.46 [95% CI: 0.96, 2.19], p = 0.07) (Table S1). Similarly, having at least one mental health provider appointment on the platform was positively, but not statistically significantly associated with a report of PPD (aOR: 1.56 [95% CI: 0.99, 2.39, p = 0.05) (Table S2).
DISCUSSION
The United States is facing a maternal mental health crisis and multi‐factorial solutions are needed to address the myriad of contributing factors to maternal mental health‐related deaths and morbidity (1). High‐risk populations such as those with a history of mental health conditions are an important target population with unique needs that may be met through digital health interventions (22). Our findings suggest the use of a combination of digital health resources is perceived as highly helpful for managing mental health among a high‐risk peripartum population. Specifically, users with a quartile increase in utilization of digital health supports were 12.5 times more likely to report better management of their anxiety and/or depression, with CA appointments, provider appointments, provider messages and article reads positively associating with better management of maternal mental health. These findings are critically important given that suicide and drug overdose are the leading causes of maternal mortality,1 and interventions that afford management of maternal mental health conditions have the potential to reduce the risk of these outcomes (7, 8). Although not statistically significant, a report of PPD was also associated with a report that Maven helped members better manage their mental health, suggesting that both those at risk for PPD and populations with PPD perceived mental health benefits from Maven utilization. These findings are consistent with prior studies demonstrating better perceived management of maternal mental health with Maven utilization (27, 28) but extend these findings to better understand the components that are driving benefits of this multi‐component digital health resource among high‐risk populations (29).
As a whole, Maven utilization among high‐risk members was not associated with an overall reduced self‐reported incidence of PPD, however our findings suggest individual components of utilization have a positive relationship to this outcome and may help guide future development and evaluation of digital peripartum mental health interventions. Though total utilization was not associated with self‐report of PPD, within the utilization mixture, provider messages and appointments, CA messages and appointments, and virtual classes showed a positive relationship with report of PPD, while article reads and class recordings showed a negative relationship with a report of PPD. These results suggest that Maven utilization is not associated with PPD, but instead, these trends likely reflect the different utilization patterns among those with current depressive symptoms and those without. For example, it is possible that those utilizing messages, appointments, and virtual classes were already experiencing symptoms of depression, as engagement in these services suggest a particular need and require more effort than reading articles and viewing recorded classes. This is further supported by our findings that users with at least one or more mental health appointments were 1.5 times more likely to report experiencing PPD. Therefore we would not expect to prevent PPD in a group that may be already experiencing depressive symptoms. Rather, we hypothesize that these resources were used in response to symptoms.
Regardless of clinical status, among this high‐risk group of peripartum people, several digital health components were associated with perceived benefit for the management of mental health. CA appointments, provider appointments, provider messages, and article reads were positively associated with perceived improvement in mental health management while virtual classes, CA messages, and class recordings are negatively associated. Overall our findings suggest that the needs of high‐risk groups may be heterogeneous and offering an array of easily accessible and readily available low‐ to higher‐intensity resources may be important in addressing maternal mental health conditions. Importantly, digital health solutions can be tailored to the individual and therefore allocates resources efficiently based on individual need, as opposed to a one‐size fits all intervention that may not be accessible to many (11, 13). Future investigations with better clinical characterization of this high‐risk population may help to inform tailored multi‐component digital health interventions that can improve management of early symptoms of PPD and/or prevent the onset of PPD (22).
The study has several strengths and limitations. Strengths of the study include a large cohort of pregnant and postpartum people at risk for PPD with assessments completed early in pregnancy and postpartum as well as well‐characterized utilization of digital health services throughout this time. We also apply a unique approach to disentangling the effects of a multi‐component digital health platform to highlight components that are potentially driving important outcomes. Limitations of our study include that members of Maven are afforded access to this platform through their employer and therefore findings may not be generalizable to unemployed populations. However, many of the demographic characteristics that associate with PPD in the broader literature (i.e., younger, parous, non‐White, living in areas with higher SVI, maternal and fetal complications) (30) are consistent with our findings and suggest that our sample is representative of those that experience PPD. Our study may also be limited due to misclassification of PPD. On average, members that endorsed PPD on their post‐delivery assessment completed this assessment at 44.7 days postpartum, compared to those that did not endorse PPD who completed their post‐delivery assessment at 18.5 days postpartum. It is possible that those in our sample without PPD may develop this condition at a later time‐point. However, the rate of PPD (∼10%) in our sample is consistent with similar studies that measure depression in the early postpartum period (30, 31). Self‐report assessments can also impact misclassification of PPD and is a limitation of the study. Misclassification due to self‐report assessment however can result in both overreporting or underreporting of PPD and therefore should not significantly impact the study findings. It is possible that participants in this sample were already experiencing depressive symptoms during pregnancy; therefore, the utilization of Maven as an intervention for PPD prevention versus disease management is obscured and is a limitation of this study. Maternal mental health symptom assessment during pregnancy using a validated scale or structured clinical interview for diagnosis is necessary to disentangle Maven utility in PPD prevention versus disease management. Similarly, assessment of comorbid psychiatric illnesses that is, psychosis, substance use disorders, and use of therapy or medications for the treatment of PPD, could help determine the utility of digital interventions in general and for specific sub‐groups. Future studies should include validated assessments and diagnostic interviews for maternal mental health symptoms and diagnoses, respectively, with longer follow‐up throughout the postpartum year.
CONCLUSIONS
Our study findings suggest digital health platforms, such as Maven, may play an important role in addressing maternal mental health problems among pregnant and postpartum people at risk for PPD. Our findings underscore the perceived maternal mental health benefits members experience when afforded accessible maternal health care through virtual platforms and illuminates components of digital healthcare that associate with meaningful outcomes. Future studies that proactively engage members in Maven supports prior to the onset of depressive symptoms are needed to determine if Maven can reduce the incidence of PPD.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31