Addressing Challenges in Residential Facilities: Promoting Human Rights and Recovery While Pursuing Functional Autonomy
Abstract
Objective
Italian residential facilities (RFs) aim to promote human rights and recovery for individuals with severe mental disorders. Italian RFs can be distinguished into five main types: high‐intensity rehabilitation (RF1), medium‐intensity rehabilitation (RF2), medium‐level support (RF3.1), high‐level support (RF3.2), low‐level support (RF3.3). This study aimed to assess the effectiveness of Italian RFs in achieving functional autonomy while upholding human rights and recovery.
Methods
Data on socio‐demographics, clinical information, patient and staff assessments of functional autonomy, types of interventions, and RF performance in various domains were collected in a pilot study with a cross‐sectional design. Descriptive and inferential analyses were conducted.
Results
Twelve RFs and 113 patients participated, with varying proportions in each RF type. RF1 patients were the oldest (p < 0.001) with the lowest functional autonomy (p < 0.001), while RF2 patients were the youngest (p < 0.001) with the lowest hospitalization rate (p < 0.001). RF3.1 patients had the highest employment rate (p = 0.024), while RF3.2 had the lowest employment rate (p = 0.024) and the longest service contact (p < 0.001). RF3.3 users had the highest functional autonomy (p < 0.001). The highest functional autonomy was in self‐care which received the highest focus in objectives and interventions. Patients rated their functional autonomy higher than professionals (p < 0.001). RFs excelled in the “human rights” and “social interface” domains but performed poorly in “recovery‐based practice,” with RF1 having the lowest performance and RF3.3 the highest.
Conclusions
This pilot study suggests that Italian RFs generally aligne with their mission and human rights principles, but personalizing interventions and implementing recovery‐oriented practices face challenges.
Highlights
Residential facilities (RFs) are not merely housing solutions but aim to help residents to be integrated into the community, and carry out significant activities in daily life.
The risk of perpetuating human rights violations and neglecting the recovery ethos remains a significant challenge in RFs.
Italian RFs generally align with their mission and human rights principles.
Challenges in Italian RFs include difficulties in personalizing interventions and implementing recovery‐oriented practices.
From the 1970s to the 1980s, the first movements in favor of the deinstitutionalization process took place worldwide, resulting in the development of different models of care (1, 2). While some countries continue to rely on hospital‐based services (3, 4, 5), others, above all in Western countries (6), have gradually reduced the number of mental hospital beds, developed community‐based care, and implemented recovery‐oriented practices. In these countries, many people with even long‐term and chronic mental health disorders live independently in the community or in accommodations with varying degrees of support, such as residential facilities (RFs) (6, 7, 8).
RFs typically cater to people with severe mental disorders (SMD) that, before deinstitutionalization, were admitted to psychiatric hospitals. People with SMD represent about 4% of people with some mental disorders, predominantly psychotic. They experience significant and enduring disruptions in their cognitive processes, emotional states, and behavior. SMDs determine complex needs for care and long‐term functioning impairment (9). They often have a profound impact on overall quality of life and are associated with marginalization from society and stigma. People with SMD need support to learn how to manage day‐to‐day tasks, as well as integration within the community (6, 10).
The aim of RFs is not to be merely housing solutions but to help residents to be integrated into the community, and carry out significant activities in daily life (10, 11).
Residential interventions should have to offer a network of relationships and opportunities to empower patients (10, 12, 13) in achieving functional autonomy (i.e., the ability to independently perform daily tasks) and personal recovery. Every patient, regardless of her/his impairment due to a psychosocial disability, deserves the opportunity to live fulfilling lives (14, 15). Residential interventions should be performed respecting human rights and reducing stigma (3, 13, 16). Successful residential interventions for people with SMD were positively associated with the adoption of recovery‐oriented practices and the promotion of human rights. Programs aimed to promote human rights, fight stigma and facilitate personal recovery may prevent the deterioration of psychosocial disabilities while simultaneously fostering an environment conducive to improved life satisfaction and functional autonomy (17, 18). However, the risk of perpetuating human rights violations and neglecting the recovery ethos remains a significant challenge in RFs (16, 19, 20). This poses a threat of exclusion from higher education and employment opportunities, poverty, social isolation, victimization, and limited access to essential physical services (21, 22).
RFs in Italy
Actually, in Italy, around 28,000 people live in RFs at a substantial cost to the Department of Mental Health (DMH) and taxpayers, representing approximately 3.6% of all patients under the care of DMH. The average number of RFs per capita is 0.7 per 10,000 inhabitants (12), which is higher compared to other high‐income European countries. According to the WHO 2020 Atlas, WHO Europe Region had more residential beds than other WHO Regions, above all in comparison with the African and the South‐East Asia Regions (5).
Italian RFs, according to the Italian Ministry of Health, can be broadly categorized into five main types (RF1 vs. RF2 vs. RF3.1 vs. RF3.2 vs. RF3.3) based on two dimensions: rehabilitation intensity and care intensity. In Table 1, Italian RFs are further categorized using the Simple Taxonomy for Supported Accommodation (STAX‐SA), which identifies different types of supported accommodations based on four domains: staffing location, level of support, emphasis on move‐on, and physical setting (23).
| Italian classification | Description | STAX‐SAb |
|---|---|---|
| High‐intensity support and high‐intensity rehabilitation | Type 2
|
| Target: Complex mental health needs, severe and unstable psychopathology, low global functioning | ||
| Aim: Stabilization of psychopathology and functioning | ||
| Staff on‐site 24/7 | ||
| Max length of stay 18 months (+6 months) | ||
| High‐intensity support and medium‐intensity rehabilitation | |
| Target: Complex mental health needs, severe and unstable psychopathology, low‐moderate global functioning | ||
| Aim: Stabilization of psychopathology and functioning | ||
| Staff on‐site 24/7 | ||
| Max length of stay 36 months (+12 months) | ||
| Medium‐intensity support and medium‐intensity rehabilitation | Type 1
|
| Target: Severe but stable psychopathology, moderate‐low global functioning | ||
| Aim: Gain community living skills | ||
| Staff on‐site 12 h a day | ||
| Max length of stay regionally established | ||
| High‐intensity support and low‐intensity rehabilitation | Type 3
|
| Target: High care needs, long‐term stable and chronic psychopathology, low global functioning | ||
| Aim: Maintenance of psychopathology and functioning | ||
| Staff on‐site 24/7 | ||
| Max length of stay regionally established | ||
| Low‐intensity support and medium‐intensity rehabilitation | Type 4
|
| Target: Stable psychopathology, moderate‐good functioning | ||
| Aim: Independence and self‐management | ||
| Visiting support few hours a day or a week | ||
| Max length of stay regionally established |
RF1 or high‐intensity rehabilitation, referrable to STAX‐SA Type 2, provides intensive therapeutic‐rehabilitative treatments with round‐the‐clock staff availability. The program has a maximum duration of 18 months, which can be extended for an additional 6 months. RF2 or Medium‐intensity rehabilitation, referred to STAX‐SA Type 2, offers extensive therapeutic‐rehabilitative treatments with staff on‐site 24/7. The program has a maximum duration of 36 months, with the possibility of extending it for another 12 months. RFs3 encompass psychosocial‐rehabilitative interventions and are categorized into three subtypes: RF3.1 or medium‐level support, referrable to STAX‐SA Type 1, provides medium‐intensity support and rehabilitation, with healthcare staff present during daylight hours (at least on weekdays). RF3.2 or high‐level support, comparable to STAX‐SA Type 3, offers round‐the‐clock presence of healthcare staff, along with sociomedical personnel available in either 24‐h or 12‐h shifts. RF3.3 or low‐level support, referrable to STAX‐SA Type 4, involves staff presence for a limited number of hours (no more than 6 h) or as needed (at least on weekdays) (13, 24).
Italian RFs represent one of the few residential settings with a well‐defined step‐progressive care pathway (6, 7, 24, 25), that is structured to facilitate the move of individuals from RFs offering high levels of support (RF1 and RF2) to those providing intermediate support (RF3.1), and eventually to facilities with minimal support (RF3.3). RF3.2 specifically provide services to residents with severe but stable mental disorders who may have limited potential for advancement to a more independent setting. In this residential system, it is essential to prioritize the admission of patients into the appropriate RFs. This ensures that they receive the most suitable care tailored to their characteristics, enabling them to progress effectively along the step‐progressive care pathway. This approach enhances the chances of promoting human rights and the recovery of the individuals within the facility (25, 26).
Only a few studies explored whether RFs embrace the personal recovery approach and promote human rights (27, 28, 29). The objective of this study was to evaluate the effectiveness of Italian RFs in fostering human rights and user recovery while actively pursuing functional autonomy. The evaluation involved examining appropriate admission practices based on functional autonomy and user characteristics, the types and objectives of residential interventions and the performance of different RFs.
METHOD
Study Design and Recruitment
The design of this study was cross‐sectional.
This study focused on RFs within the Verona DMH (ex ULSS 20 area), an area which has previously been shown to be comparable to the Italian mental health population (7, 12). This area underwent a quality‐of‐care improvement program from 2015 to 2019. The program aimed to reorganize and enhance the Verona DMH RFs, facilitating proper admission and stay monitoring for residents. To achieve this goal, experts in Italian RFs developed the tool named Monitoring of the Path of Rehabilitation Form (MPR) in 2014 with a bottom‐up approach. After a pilot study from 2015 to 2019, collaborative efforts led to the MPR's refinement and validation in 2022 (30). This tool addressed a gap in Italian mental health care by assessing functional autonomy in RFs, aiding in placement decisions and goal setting.
Inclusion criteria for patients in the pilot study were: residing in one RFs of ex ULSS 20 area by 6 months (this timeframe coincided with the point at which residents typically undergo assessments of their stay) between May 2016 and November 2018; being under the care of the Verona DMH; having a primary diagnosis of psychiatric disorder according to DSM‐5; more than 18 y.o.; adequate understanding of the Italian language. The exclusion criterion was the inability to provide informed consent (e.g. because of low education or cognitive impairment).
Written informed consent was obtained from all participants.
Assessments
Socio‐demographic and clinical data were collected by researchers. Standardized tools, described below, were completed by RF staff members, senior managers and residents. All participants, except for residents, were previously trained in the use of the tools.
Residents' Evaluations
Socio‐demographic and clinical data were collected for each patient through the Verona DMH dataset and the Verona South RPC (31).
Functional autonomy was assessed with the MPR (30), constituted by 40 items grouped into 10 basic skills (self‐care, care of living space, feeding, orientation/movement, other autonomies [money, cigarettes, free time], relational skills, social‐recreational skills, occupational‐work skills, physical health management, and mental health management), rated on a 4‐point‐Likert scale ranging from 0 (“not autonomous”) to 3 (“autonomous”). Five stages of functional autonomy are recognized according to the mean score: poor (0–2.3), mediocre (2.4–4.7), fair (4.8–7.1), good (7.2–9.5), and excellent (9.6–12.0). The MPR was completed by both staff MPR‐S (Staff Assessment) and MPR‐U (User/patient Assessment). According to its validation, MPR inter‐rater and test‐retest reliability were good, as well for concurrent validity and acceptability.
Residential Interventions
Main goals of residential interventions were collected through the MPR, which includes a specific section dedicated to formulating a treatment plan with SMART goals (Specific, Measurable, Attainable, Relevant, Timely) (32). These goals are defined based on the MPR‐S and MPR‐U scores.
Type of residential interventions provided in RF was collected using the Activity and Intervention Log Form, a document part of the MPR that on a daily basis gathers 59 interventions/activities grouped into 16 categories [support in cooking/cleaning/corvé, medication administration, support money/cigarettes management, rehabilitative‐occupational activities, leisure activities, support in crisis, contacts and/or groups with family members, internal service users' meeting, meeting with others (e.g. support workers), meeting with the community team, internal staff meeting, meeting with a psychiatrist, psychological intervention (meeting and/or group), users' self‐help meeting, shopping support].
RFs Performance
Performance of RFs was assessed using the QuIRC‐SA (The Quality Indicator for Rehabilitative Care–Supported Accommodation; https://quirc.eu/quirc‐sa/) (33), that, completed by a senior manager, comprises 143 items, out of which 55 provide descriptive information on service characteristics, while the remaining 88 contribute to the scoring of seven domains (living environment, therapeutic environment, treatments and interventions, self‐management and autonomy, social interface, human rights, and recovery‐based practice) that assess various aspects of the quality of care in a recovery perspective. The quality of each domain is assessed as a percentage, where higher scores indicate better quality.
Statistical Analysis
Data were presented as frequencies, means, standard deviations and percentages.
The comparison of MPR scores, objectives and interventions/activities (collected using the Activity and Intervention Log Form data in the 6 months before the MPR‐S completion) among the different types of RFs (RF1 vs. RF2 vs. RF3.1 vs. RF3.2 vs. RF3.3) was done using the t‐test for independent samples. For continuous variables, Bonferroni's post hoc test was performed.
The comparison of scores on the MPR‐S and the MPR‐U was done using the paired‐sample t‐test.
All tests were two‐sided with a significance level of 0.05.
Statistical analyses were performed using the Stata 13 programme.
RESULTS
Enrolled Sample
This study involved 12 (40.0%) RFs (ex ULSS 20) out of the 30 RFs of the Verona DMH. In detail, RFs were 2 (16.6%) RF1, 3 (25.1%) RF2, 3 (25.1%) RF3.1, 2 (16.6%) RF3.2 and 2 (16.6%) RF3.3.
Twenty‐six patients were excluded because they did not give their informed consent (3 patients) or dropped out (13 patients). One‐hundred thirteen patients were assessed, whose 22 (19.5%) were residents in RF1, 35 (31.0%) in RF2, 22 (19.5%) in RF3.1, 24 (21.2%) in RF3.2 and 10 (8.8%) in RF3.3.
Fifty‐nine (93.7%) staff members out of 63 staff members of all RFs participated in the study.
Eleven (91.7%) RF senior managers out of 12 RFs senior managers participated in the study.
Residents' Socio‐Demographic and Clinical Characteristics
As shown in Table 2, patients had a mean age of 50.5 (SD = 10.8) years and were mostly males (63.7%), single (84.0%), and unemployed (71.7%). Most had a principal diagnosis of schizophrenia spectrum disorder (62.2%) and an average of 25.7 (SD = 11.9) years of contact with mental health services.
| RF1 | RF2 | RF3.1 | RF3.2 | RF3.3 | Total | pb | Bonferroni | |
|---|---|---|---|---|---|---|---|---|
| 24 patients (21.2%) | 35 patients (31.0%) | 22 patients (19.5%) | 22 patients (19.5%) | 10 patients (8.8%) | 113 patients (100.0%) | |||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |||
| Gender, M | 13 (54.2%) | 21 (60.0%) | 18 (81.8%) | 14 (63.6%) | 6 (60.0%) | 72 (63.7%) | 0.303 | ‐ |
| Age, mean (SD) | 57.2 (8.8) | 43.7 (9.7) | 49.3 (11.9%) | 56.4 (5.1) | 48.2 (10.9) | 50.5 (10.8) | <0.001 | RF2 < RF3.2/RF1 |
| Marital status | ||||||||
| Never married | 18 (78.3%) | 32 (94.1%) | 17 (81.0%) | 17 (81.0%) | 5 (71.4%) | 89 (84.0%) | 0.290 | ‐ |
| Currently married/cohabitated | 3 (13.0%) | 2 (5.9%) | 1 (4.8%) | 2 (9.5%) | 0 (0.0%) | 8 (7.5%) | ||
| Widowed/separated/divorced | 2 (8.7%) | 0 (0.0%) | 3 (14.3%) | 2 (9.5%) | 2 (28.6%) | 9 (8.5%) | ||
| (23 patients) | (34 patients) | (21 patients) | (21 patients) | (7 patients) | (106 patients) | |||
| Education | ||||||||
| Low education (primary school, secondary school) | 14 (63.6%) | 21 (74.2%) | 15 (75.0%) | 17 (18.7%) | 6 (85.7%) | 73 (74.5%) | 0.554 | ‐ |
| High education (high school, degree) | 8 (36.4%) | 8 (25.8%) | 5 (25.0%) | 3 (15.0%) | 1 (14.3%) | 25 (25.5%) | ||
| (22 patients) | (29 patients) | (20 patients) | (20 patients) | (7 patients) | (98 patients) | |||
| Working status | ||||||||
| Employed | 8 (33.3%) | 7 (20.0%) | 10 (45.5%) | 3 (14.0%) | 4 (40.0%) | 32 (28.3%) | 0.024 | RF3.2 < RF3.1/RF3.3 |
| Unemployed or looking for a job | 9 (37.5%) | 16 (45.7%) | 12 (54.5%) | 8 (36.0%) | 1 (10.0%) | 46 (40.7%) | ||
| Other (e.g. retired, housewife, student, voluntary work) | 7 (29.2%) | 12 (34.3%) | 0 (0.0%) | 11 (50.0%) | 5 (50.0%) | 35 (31.0%) | ||
| Physical comorbidity | 5 (41.7%) | 7 (41.2%) | 8 (47.1%) | 4 (40.0%) | 1 (33.3%) | 25 (42.4%) | 0.323 | ‐ |
| (12 patients) | (17 patients) | (17 patients) | (10 patients) | (3 patients) | (59 patients) | |||
| Primary psychiatric diagnosis | ||||||||
| Schizophrenia spectrum disorders | 16 (69.6%) | 25 (71.4%) | 8 (36.4%) | 15 (71.4%) | 5 (50.0%) | 69 (62.2%) | 0.061 | ‐ |
| Bipolar syndrome | 5 (21.7%) | 2 (5.7%) | 2 (9.1%) | 0 (0.0%) | 2 (20.0%) | 11 (9.9%) | ||
| Depressive disorders and anxiety | 0 (0.0%) | 3 (8.6%) | 2 (9.1%) | 2 (9.5%) | 1 (10.0%) | 8 (7.2%) | ||
| Personality disorders | 0 (0.0%) | 2 (5.7%) | 5 (22.7%) | 3 (14.3%) | 0 (0.0%) | 10 (9.0%) | ||
| Other | 2 (8.7%) | 3 (8.6%) | 5 (22.7%) | 1 (4.8%) | 2 (20.0%) | 13 (11.7%) | ||
| (23 patients) | (21 patients) | (111 patients) | ||||||
| Contact with mental health services (years) mean (SD) | 31.2 (10.2) | 19.4 (10.7) | 22.0 (10.3) | 34.8 (8.2) | 14.5 (8.3) | 25.7 (11.9) | <0.001 | RF3.3/RF2/RF3.1 < RF1/RF3.2 |
| (23 patients) | (24 patients) | (20 patients) | (20 patients) | (6 patients) | (96 patients) | |||
| Lifetime previous admissions, mean (SD) | 8.2 (12.7) | 0.89 (2.0) | 3.7 (7.7) | 6.4 (11.5) | 0.67 (2.0) | 4.1 (8.9) | 0.013 | RF2 < RF1 |
| (9 patients) | (112 patients) | |||||||
| Previous lifetime involuntary admissions | 10 (50.0%) | 3 (10.7%) | 4 (23.5%) | 6 (33.3%) | 1 (25.0%) | 24 (27.6%) | 0.050 | RF2 < RF1 |
| (20 patients) | (28 patients) | (17 patients) | (18 patients) | (4 patients) | (87 patients) | |||
Patients in RF1 were the oldest (p < 0.001) with the highest number of lifetime voluntary (p = 0.013) and involuntary (p = 0.050) admissions. RF2 patients were the youngest (p < 0.001) with the lowest number of lifetimes acute ward admissions (p = 0.050). RF3.1 patients had the highest occupancy rate (p = 0.024) and the lowest number of diagnoses of schizophrenia spectrum disorder (n.s.). Residents in RF3.3 had the fewest years of contact with mental health services (p < 0.001). RF3.2 residents had the lowest occupancy rate (p = 0.024) and the highest number of years of contact with mental health services (p < 0.001) (Table 2).
Functional Autonomy of Residents Across RFs
As shown in Table 3, residents presented a fair functional autonomy (mean total score 6.8, SD = 2.3) according to staff members. The best functional autonomy was in orientation/movement (8.0, SD = 4.0) and Self‐care (8.1, SD = 3.5), while the worst was in occupational‐work skills (4.5, SD = 2.9) and mental health management (4.9, SD = 3.3).
| RF1 | RF2 | RF3.1 | RF3.2 | RF3.3 | Total | pb | Bonferroni | |
|---|---|---|---|---|---|---|---|---|
| 24 patients (21.2%) | 35 patients (31.0%) | 22 patients (19.5%) | 22 patients (19.5%) | 10 patients (8.8%) | 113 patients (100.0%) | |||
| 1. Self care | 6.2 (3.8) | 9.1 (3.1) | 8.5 (3.2) | 7.1 (3.1) | 11.1 (1.6) | 8.1 (3.5) | <0.001 | RF3.2 < RF3.3 |
| (33 patients) | (111 patients) | |||||||
| 2. Care of living space | 4.9 (3.8) | 8.4 (3.0) | 7.1 (2.8) | 5.0 (2.8) | 8.3 (3.5) | 6.7 (3.5) | <0.001 | RF3.2/RF1 < RF2 |
| 3. Feeding | 7.2 (2.7) | 7.1 (2.5) | 7.8 (2.5) | 6.2 (2.3) | 8.3 (2.9) | 7.2 (2.6) | 0.197 | ‐ |
| (9 patients) | (112 patients) | |||||||
| 4. Orientation/movement | 6.0 (5.4) | 8.7 (3.5) | 8.7 (3.4) | 6.7 (3.3) | 10.8 (1.5) | 8.0 (4.0) | 0.004 | RF3.2/RF1 < RF3.3 |
| (22 patients) | (33 patients) | (109 patients) | ||||||
| 5. Other autonomies | 4.8 (4.4) | 6.2 (3.2) | 7.0 (3.2) | 5.6 (3.6) | 8.5 (2.7) | 6.1 (3.6) | 0.055 | RF1 < RF3.3 |
| (21 patients) | (112 patients) | |||||||
| 6. Relational skills | 6.9 (4.5) | 7.4 (2.9) | 8.2 (2.8) | 7.2 (3.5) | 7.8 (3.4) | 7.4 (3.4) | 0.733 | ‐ |
| (21 patients) | (112 patients) | |||||||
| 7. Social‐recreational skills | 5.6 (4.0) | 6.5 (3.2) | 7.6 (3.2) | 4.9 (3.5) | 7.6 (3.7) | 6.3 (3.6) | 0.082 | ‐ |
| (21 patients) | (9 patients) | (111 patients) | ||||||
| 8. Occupational‐work skills | 2.6 (2.1) | 4.6 (2.4) | 6.4 (3.1) | 3.2 (1.8) | 7.3 (3.3) | 4.5 (2.9) | <0.001 | RF1 < RF3.3 |
| (9 patients) | (112 patients) | |||||||
| 9. Physical health management | 6.7 (3.8) | 8.1 (3.2) | 8.4 (2.7) | 7.0 (3.4) | 9.8 (2.9) | 7.8 (3.3) | 0.073 | ‐ |
| (20 patients) | (111 patients) | |||||||
| 10. Mental health management | 4.0 (3.6) | 5.7 (3.0) | 3.7 (3.0) | 4.1 (2.7) | 8.1 (2.8) | 4.9 (3.3) | 0.001 | RF1 < RF3.3 |
| (34 patients) | (19 patients) | (109 patients) | ||||||
| Total mean score | 5.4 (3.0) | 7.1 (2.0) | 7.7 (1.4) | 5.9 (1.7) | 8.8 (1.9) | 6.8 (2.3) | <0.001 | RF1/RF3.2 < RF2/RF3.1/RF3.3 |
| (21 patients) | (31 patients) | (20 patients) | (10 patients) | (9 patients) |
Residents with the lowest functional autonomy were in RF1 (mean total score 5.4, SD = 3.0), while residents of RF3.3 presented the highest one (mean total score 8.8, SD = 1.9) (p < 0.001). In detail, RF1 users showed significantly lower functional autonomy than RF3.3 users in orientation/movement (p = 0.004), Other autonomies (p = 0, 055), Occupational‐work skills (p < 0.001), and Mental health management (p = 0.001). RF1 users showed also significantly lower autonomy in the Care of Living Space than the RF2 (p < 0.001) (Table 3). RF3.3 residents showed significantly greater functional autonomy compared to RF3.2 users in Self‐care (p < 0.001) and orientation/movement (p = 0.004).
The RF3.2 patients were the second group of residents of the sample with the lowest functional autonomy (total mean score 5.9, SD = 1.7). RF2 and RF3.1 residents showed fair functional autonomy (respectively mean total score 7.1, SD = 2.0 and 7.7, SD = 1.4) (Table 3).
Forty‐four (38.9%) patients of the sample completed the MPR‐U. As shown in Table S1, these 44 MPR‐U were compared to the corresponding 44 MPR‐S filled in by staff members for the same patient. The analysis of total functional autonomy, as assessed by both professionals and patients, revealed a significant difference (p < 0.001). Residents consistently reported higher levels of functional autonomy (approximately >2 points) in all dimensions, except for orientation/movement.
SMART Goals of Residential Interventions
SMART goals were established to be achieved in approximately two‐thirds (68.2%) of the sample cases. Goals were mostly about Self‐care (80.5%) and Care of the living space (77.0%), while in the minority of cases they were about Physical health (56.6%) and Mental health management (58.4%) (Table S2).
The lowest number of goals was set for RF3.3 users and the highest for RF3.2 residents (p < 0.001). RF1 and RF2 users showed the highest significant number of goals set in Self‐care (p < 0.001) compared to RF3.3 residents, and in Feeding (p = 0.001) and Social skills (p = 0.010) compared to RF3.1 residents. The lowest number of goals was in orientation/movement (60.0%) and Physical health management (60.0%) in RF2 residents and mental health management (41.7%) and occupational‐work skills (50.0%) in RF1 residents (Table S2).
Types of Residential Interventions
As shown in Table 4, the number of residential interventions, carried out in all RFs in the 6 months before the MPR completion and collected using the Activity and Intervention Log Form, was 774.0 (SD = 513.6) (4.2 activities/day). The highest number was for the support in cooking/cleaning/corvé (345.7 interventions/semester, SD = 282.4) (1.9 times/day) followed by medication administration (279.2 interventions/semester, SD = 232.3) (1.5 times/day), while the lowest number of activities was recorded in meetings among users outside facilities (1.4 interventions/semester, SD = 2.5) (3 times/year), psychological interventions (1.5 interventions/semester, SD = 3.6) (3 times/year) and shopping support (0.5 interventions/semester, SD = 1.4) (1 time/year).
| RF1 | RF2 | RF3.1 | RF3.2 | RF3.3 | Total | pb | Bonferroni | |
|---|---|---|---|---|---|---|---|---|
| 24 patients (21.2%) | 35 patients (31.0%) | 22 patients (19.5%) | 22 patients (19.5%) | 10 patients (8.8%) | 113 patients (100.0%) | |||
| Support in cooking/cleaning/corvé | 450.7 (217.0) | 282.9 (234.8) | 76.3 (95.0) | 521.6 (345.2) | 72.0 (66.5) | 345.7 (282.4) | <0.001 | RF3.2 > RF3.3 |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Medication administration | 262.7 (155.5) | 302.4 (275.2) | 101.3 (92.6) | 391.4 (261.6) | 188.0 (22.6) | 279.2 (232.3) | 0.051 | RF3.2 < RF3.1 |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Support money/cigarettes management | 178.8 (381.8) | 111.2 (55.7) | 49.7 (51.4) | 110.6 (165.8) | 72.0 (17.0) | 120.3 (217.8) | 0.675 | |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Rehabilitative‐occupational activities | 103.3 (86.7) | 185.6 (171.1) | 36.3 (42.8) | 13.1 (13.7) | 99.0 (32.5) | 102.3 (128.9) | 0.042 | RF2 < RF3.2 |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Leisure activities | 5.6 (6.8) | 28.6 (42.8) | 23.2 (36.8) | 4.8 (4.2) | 45.5 (51.6) | 16.9 (31.2) | <0.001 | ‐ |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Support in crisis | 23.8 (42.4) | 12.3 (24.0) | 12.3 (16.4) | 0.0 (0.0) | 12.0 (8.5) | 12.9 (27.8) | 0.214 | |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Contacts and/or groups with family members | 13.0 (11.5) | 12.2 (16.0) | 11.9 (16.5) | 2.5 (3.0) | 13.5 (9.2) | 10.3 (13.2) | 0.173 | ‐ |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Internal service users' meeting | 2.6 (2.8) | 12.2 (7.4) | 1.0 (1.7) | 4.8 (3.9) | 3.5 (5.0) | 6.1 (6.7) | <0.001 | RF3.1 < RF2 |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Meeting with others (e.g. support workers) | 7.7 (7.6) | 6.3 (14.1) | 4.7 (5.1) | 0.9 (1.2) | 27.5 (36.1) | 5.9 (11.2) | 0.024 | RF3.2 < RF3.3 |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Meeting with the community team | 1.6 (1.4) | 10.9 (15.9) | 5.6 (7.9) | 0.0 (0.0) | 20.0 (17.0) | 5.5 (11.1) | 0.004 | RF3.2 < RF3.3 |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Internal staff meeting | 2.0 (2.3) | 11.2 (15.7) | 1.4 (2.3) | 0.0 (0.0) | 19.0 (15.6) | 5.1 (10.8) | 0.001 | RF3.2 < RF3.3 |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Meeting with a psychiatrist | 0.5 (0.8) | 3.1 (4.2) | 2.8 (3.5) | 0.1 (0.5) | 8.0 (2.8) | 1.8 (3.3) | 0.001 | RF3.2 < RF3.3 |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) | |||
| Psychological intervention (meeting and/or group) | 1.0 (1.2) | 2.3 (3.3) | 2.9 (6.9) | 0.0 (0.0) | 0.0 (0.0) | 1.5 (3.6) | 0.260 | ‐ |
| (8 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (55 patients) | |||
| Users' self‐help meeting | 1.6 (3.3) | 1.3 (1.1) | 2.2 (3.3) | 0.4 (0.8) | 5.5 (6.4) | 1.4 (2.5) | 0.071 | |
| (18 patients) | (21 patients) | (9 patients) | (14 patients) | (2 patients) | (64 patients) | |||
| Shopping support | 0.1 (0.2) | 0.6 (1.3) | 2.3 (2.6) | 0.0 (0.0) | 0.5 (0.7) | 0.5 (1.4) | 0.001 | RF3.2 < RF2/RF3.3 < RF3.1 |
| (18 patients) | (22 patients) | (8 patients) | (14 patients) | (2 patients) | (64 patients) | |||
| Total mean (mean of the sum of all activities/interventions) | 847.2 (413.4) | 845.3 (527.6) | 266.4 (219.8) | 934.4 (599.5) | 492.5 (170.4) | 774.0 (513.6) | 0.016 | RF3.1 < RF2/RF1 < RF3.2 |
| (18 patients) | (22 patients) | (9 patients) | (14 patients) | (2 patients) | (65 patients) |
The highest number of residential interventions was carried out in RF3.2 (934.4 interventions/semester, SD = 599.5) (2.5 times/day), while the lowest in RF3.1 (266.4 interventions/semester, SD = 219.8) (0.7 times/day) (p = 0.016). RF2 was the RF with the highest number of activities related to rehabilitative‐occupational activities, especially compared to RF3.2 (p = 0.042). The RF3.1 showed the highest number of activities related to shopping support, especially compared to RF3.2 (p = 0.001), and the lowest number of user meetings in the RF, especially compared to the RF2 (p < 0.001). The RF3.2 showed a significantly higher number of activities compared to the RF3.3 regarding support in cooking/cleaning/corvé (p < 0.001), while it showed a lower number of activities compared to RF3.3 regarding interviews with a psychiatrist (p < 0.001) and with other professionals (p = 0.024), internal staff meetings (p = 0.001) and meetings with the community team (p = 0.004) (Table 4).
RFs Performance
Out of the 11 RF senior managers who took part in the study, the completion of the QuIRC‐SA was as follows: one (9.1%) completed for RF1, three (27.3%) completed for RF2, three (27.3%) completed for RF3.1, two (18.2%) completed for RF3.2, and two (18.2%) completed for RF3.3.
Information collected using QuIRC‐SA from RFs managers shows that on a range of performance from 0% (minimum) to 100% (maximum), overall, the worst performance was in the “recovery‐based practice” domain (42.4%, SD = 10.6) while the best performance was in “human rights” (56.2%, SD = 13.0) and “social interface” domains (56.4%, SD = 18.5). RF1 presented the overall worst performance (41.6%), while RF3.3 the best one (63.0%) (Figure 1 and Table S3).
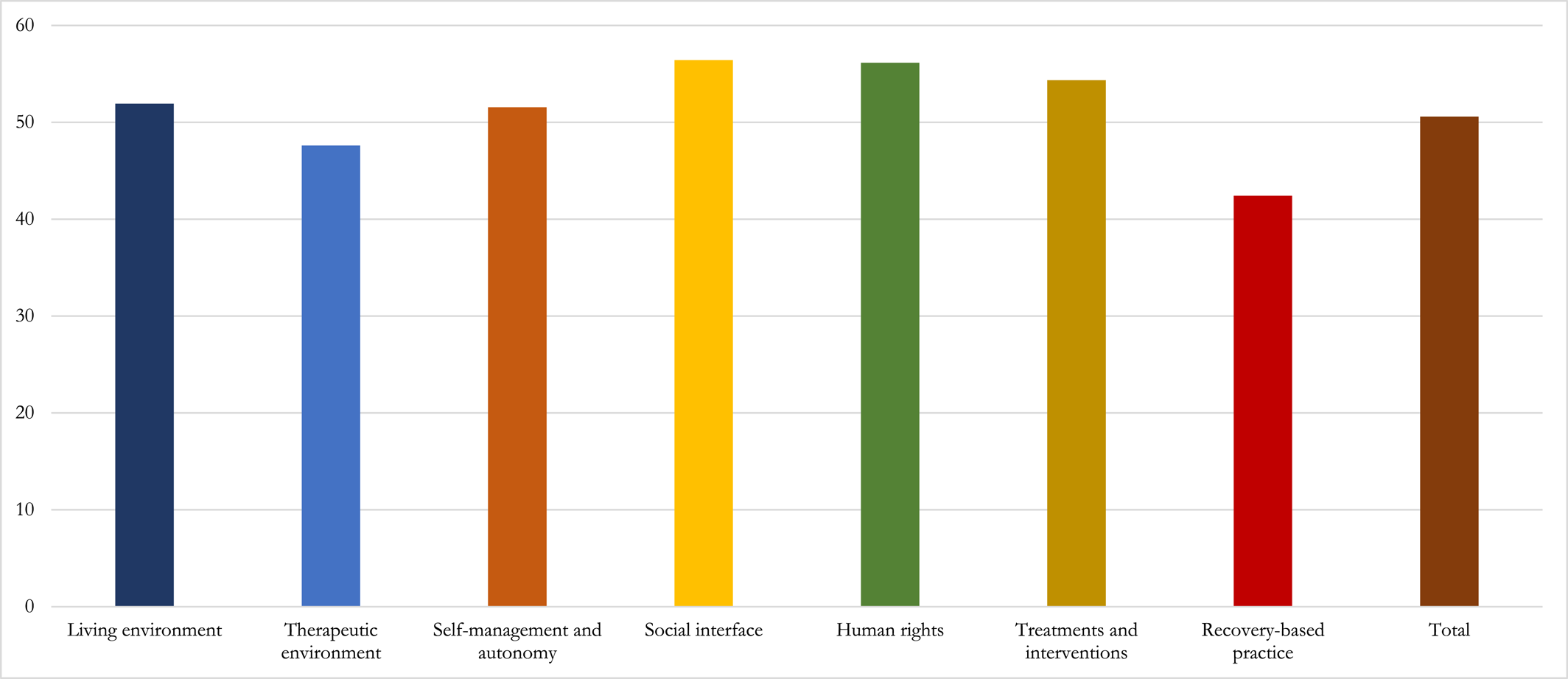
FIGURE 1. Quality of the performance of Italian RFs in each QuIRC‐SA domain. QuIRC‐SA, Quality Indicator for Rehabilitative Care–Supported Accommodation; RFs, residential facilities.
DISCUSSION
This study represents the first investigation in Italy aimed at exploring the effectiveness of Italian RFs in promoting human rights and user recovery, while actively pursuing functional autonomy.
According to the collected data, we can distinguish a different patient profile for each RF:
The oldest patients of the sample with a high number of admissions, fair functional autonomy (the worst of the whole sample) in high‐intensity rehabilitation RF (RF1);
The youngest patients of the sample with few years of contact with mental health services, a low number of hospitalizations, fair (towards good) functional autonomy in high‐intensity rehabilitation RF (RF2);
Patients with a mean age and the highest rate of employment and fewer diagnoses of psychosis, good functional autonomy in medium‐level support RF (RF3.1);
The second group of the oldest patients of the sample with the most years of contact with services, mediocre functional autonomy in high‐level support RF (RF3.2);
Patients in the mean age of the sample with good functional autonomy (the best of the whole sample) in low‐level support RF (RF3.3).
These findings corroborate data from previous research (25, 29) that indicates that residents were mostly adequately admitted to RFs. However, our findings indicate that high‐intensity rehabilitation RF (RF1) falls short of fulfilling its intended role of providing what is necessary for the first step of the care pathway. While other RFs of the care pathway (RF2, RF3.1, and RF3.3) provide residential interventions that reflect a commitment to enhancing residents' skills, RF1 residential interventions seem to be less oriented to increase the patients' functional autonomy. Nevertheless, RF1 QuIRC‐SA scores resulted in the lowest. These results shed light on potential shortcomings in the admission practices within RF1. This may be partly due to the specific timeframe of data collection when an organizational transition was supposed to move patients from RF1 to high‐level support RF (RF3.2) or nursing homes.
Our findings highlight a low specificity of residential interventions. A significant emphasis was placed on interventions targeting basic autonomy skills, such as self‐care, rather than addressing more subjective and personal domains, such as mental health or social management, or work/occupational domains. This is particularly noteworthy as patients demonstrated lower functional autonomy in these specific areas. This finding is consistent with previous research (28, 34), as interventions targeting basic autonomy skills are comparatively easier to implement, as they typically involve practical and tangible tasks, and are often prioritized due to the challenges associated with motivating individuals with SMD to engage in self‐care practices (28, 35).
Furthermore, the discrepancy between patient and staff members evaluations on MPR may be explained by patients' overestimation of their abilities, a common occurrence with self‐assessment tools (36), and professionals' underestimation of patients' functional autonomy due to a paternalistic view and a possibly stigmatized perceptions of patients (25).
The QuIRC‐SA results align with broader previous Italian research (25, 29). They highlight factors such as RFs' commitment to respecting human rights, their challenges in achieving their primary goal of establishing a supportive network of relationships for residents (13), and the imperative need to implement the recovery approach, which received the lowest score in the QuIRC‐SA assessment. These findings suggest that Italian mental health professionals may face challenges in overcoming paternalistic practices that impede progress and restrict expectations (37, 38) and in grasping the concept of personal recovery (10).
The QuIRC‐SA domain scores in our study typically scored lower, with the exception of the treatments and interventions domain, when compared to a national sample of mental health supported accommodation services in England. This national sample, which is the only comparable study (39), had an average score of 68.3%, ranging from 54.2% (SD = 8.1) in treatments and interventions to 85.5% (SD = 6.9) in human rights.
We acknowledge several limitations of our study that should be taken into consideration.
Firstly, there may be some data inaccuracies in the Activity and Intervention Register Log due to potential underreporting by mental health professionals. This could occur if professionals were not consistently present in the RFs or if patients failed to report certain activities, leading to missing data and potential errors.
Secondly, the study would have benefitted from a larger number of RFs (QuIRC‐SA completion) and residents to enhance the representativeness of Verona RF patients. Nevertheless, the evaluations conducted were generally meticulous, allowing for a reliable investigation of the study's objectives.
Furthermore, it is important to note the absence of data regarding the severity of psychopathological symptoms and the specific needs for care of the residents. Such information could have provided valuable insights for data interpretation and analysis.
Lastly, the cross‐sectional design of the study presents limitations in establishing causality between the associated variables.
This study represents the first attempt in Italy to investigate the adequacy of residential interventions in different types of Italian RFs in promoting and respecting human rights and recovery while pursuing patients' functional autonomy.
This study findings suggested the adherence of Italian RFs to human rights principles and the facilitation of social networks within the community. Although most patients were adequately admitted to RFs based on their characteristics and functional autonomy, not all RFs fully align with their specific mission. The personalization of residential interventions and the implementation of recovery‐oriented practices still pose challenges in Italian RFs.
To foster a more supportive and empowering environment within Italian RFs, it is crucial to prioritize staff training in rehabilitation interventions that embrace the principles of personal recovery (40, 41). Conducting pilot studies and longitudinal research focused on a recovery‐oriented approach will further advance our understanding (42).
By implementing these efforts, we can enhance the effectiveness and appropriateness of residential interventions in Italian RFs, promoting the recovery, functional autonomy, and human rights of individuals with mental health disorders while preventing psychosocial disability.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42