Adapting Virtual Reality‐Based Mental Health Interventions for Equitable Global Use: Proof of Concept
Among low and middle‐income countries (LMICs), mental health challenges are compounded by poverty and limited access to mental health services, particularly among older adults (1, 2, 3). There is a need for effective and innovative interventions tailored to these populations. Mindfulness interventions can be applied trans‐diagnostically and have been shown as feasible and effective in LMICs (4).
However, mindfulness can be challenging to engage with, especially at the start of the practice (5). Notably, minoritized and disadvantaged populations tend to engage less in mindfulness (6), and older adults may also have difficulty with these interventions (7). One approach to improving the effectiveness of mindfulness among older adults may be by using virtual reality (VR). VR has been shown to facilitate a greater state of mindfulness when compared to audio‐only mindfulness interventions (8).
Low‐cost VR hardware and expanding content availability may facilitate their implementation to older adults in LMICs. In this study, we aimed to demonstrate whether a manualized low‐cost VR mindfulness intervention is feasible, tolerable, and effective among older adults with and without mild cognitive impairment (MCI) in Quito, Ecuador. This feasibility study has significant implications for determining the scalability of mindfulness‐based interventions as well as for demonstrating how advanced technologies like VR can be made much more accessible.
METHODS
We conducted 10 weekly sessions of VR‐assisted mindfulness for older adults in Quito, Ecuador. This study was approved by the Institutional Review Board at Universidad San Francisco de Quito. The study used low‐cost VR DesTeK VS VR headsets (costing $70) requiring a smartphone to run VR apps. For this study, we specifically selected the free and publicly available “Sites in VR” application as it offers a variety of static nature scenes ideal for guided meditation. This approach leverages the widespread use of smartphones in LMICs (9) and removes the need for WIFI or more complex VR headsets.
We recruited 28 older adults ages 61 or older with subclinical anxiety and depression through social media. Inclusion criteria were normal cognitive functioning or MCI determined using the Montreal Cognitive Assessment (MoCA), being able to give written consent, and being a Spanish speaker. The MoCA cut‐off score was set at 26 based on the original MoCA and the use of the Spanish MoCA in other Latin American countries (10). Exclusion criteria were moderate to severe cognitive impairment, blindness or severe vision problems, deafness or hearing problems, history of dizziness, and current psychosis or mania.
Tailoring the Intervention for the Study Population and Location
We used a Spanish‐translated standardized mindfulness script to deliver the mindfulness intervention. We elected to use static 360° VR content using the “Sites in VR” app. Because the gyroscope sensor required to use the VR headset is not always available in smartphones sold in Latin America, we used devices obtained in the United States. Gyroscope sensors allow the mobile device to detect and measure an individual's orientation, rotational movement, and the position of the device in space. These sensors are essential for full immersion in the VR environment. Following the conclusion of the study, all devices were returned to study staff.
Intervention Sessions
We offered participants a choice between home visits or clinic visits to include those with transportation issues. Nineteen participants preferred home visits, and nine attended clinic visits. In each session, we selected a nature scene from the “Sites in VR” app, then placed the smartphone in the headset and adjusted the fit for each participant. Participants were seated while using the headset to minimize the risk of falls, accidents, and motion sickness while eliminating the need for hand controllers to “move” in the virtual space.
We delivered a practical form of Acceptance and Commitment Therapy using guided visualization to emphasize the principles of cognitive diffusion and emotional acceptance (11, 12). In each 45‐min session, the therapist guided participants through a nature scene in VR for 15 min. Participants were asked to imagine what they were smelling, hearing, touching, and tasting while in the VR environment to facilitate full immersion in the experience. Study participants were also prompted to imagine how moving around the VR environment might feel. Processing and debriefing sessions followed the exercise. All sessions were video and audio recorded to ensure consistency and to assess participants' responses.
Outcomes
Attrition and Acceptability
We documented attrition and reasons for dropout and used standardized open‐ended questions to document experiences after every intervention session and any physical symptoms or discomfort.
If participants reported dizziness when asked about general discomfort, we administered the Spanish version of the Dizziness Handicap Inventory (DHI).
Clinical Outcomes
Though our population was subclinical, we evaluated anxiety and depression symptoms to evaluate the general impact on psychological health, using the Spanish versions of the Geriatric Depression Scale (GDS‐15) (13) and the Generalized Anxiety Disorder (GAD‐7) (14). In addition, we assessed perceived stress, trait mindfulness, and behavior activation using Spanish versions of the Perceived Stress Scale (PSS) (15), the Mindfulness Attention Awareness Scale (MAAS) (16), and the Behavioral Activation Scale for Depression (BADS) (17). All the scales were administered at three time points: pre‐screening, post‐intervention, and 1‐month post‐intervention. We used the MoCA (18) scores to assess cognitive status.
Statistical Analysis
We applied a Bonferroni Correction to set the p‐value cut‐off for significance at 0.00 and tested the normality of the data using the Shapiro‐Wilk test. For scales that were not normally distributed (GAD and GDS), we used the Wilcoxon Signed Ranked test to examine changes from pre‐ to post‐intervention and 1‐month follow‐up. We used linear mixed models with random intercept to examine changes across time points for normally‐distributed outcome data (PSS, BADS, and MAAS).
RESULTS
Attrition and Acceptability
We recruited a total of 28 older adults aged 61 to 81. The minimum age to participate was 61, but there was no upper cut‐off. The average age of our sample was 68 years (SD = 6.5) and women (N = 22) comprised the majority. Six participants (21%) dropped out over the course of the study: five were for reasons unrelated to the study, and one discontinued study participation after the third intervention session due to dizziness and discomfort with the VR headset, Accordingly, study staff administered the DHI to this participant. No other participants reported physical symptoms during the intervention.
Our sample was highly educated with all participants reporting at least a high school degree and 21 reporting an undergraduate degree or higher. The majority of our sample (N = 25) identified as “Mestizo,” a person of mixed European and indigenous background, three identified as White, and 13 reported being married. Seventeen (60%) of the participants had MoCA scores at or below 26, suggesting MCI.
Only three participants had a formal diagnosis of a depressive or anxiety disorder and none were receiving any additional psychological or psychiatric treatment at the time of study participation. The data of all participants were pooled for analyses as all participants completed the same intervention and outcome measures.
Psychological Measures
We noted that GDS scores significantly decreased using the Wilcoxon Signed ranked test pre‐ to post‐intervention, and pre‐ to 1‐month follow‐up (see Figure 1 and Table 1). We did not find a significant change in GAD‐7 scores but there was a trend reduction from pre‐intervention to 1 month follow‐up.
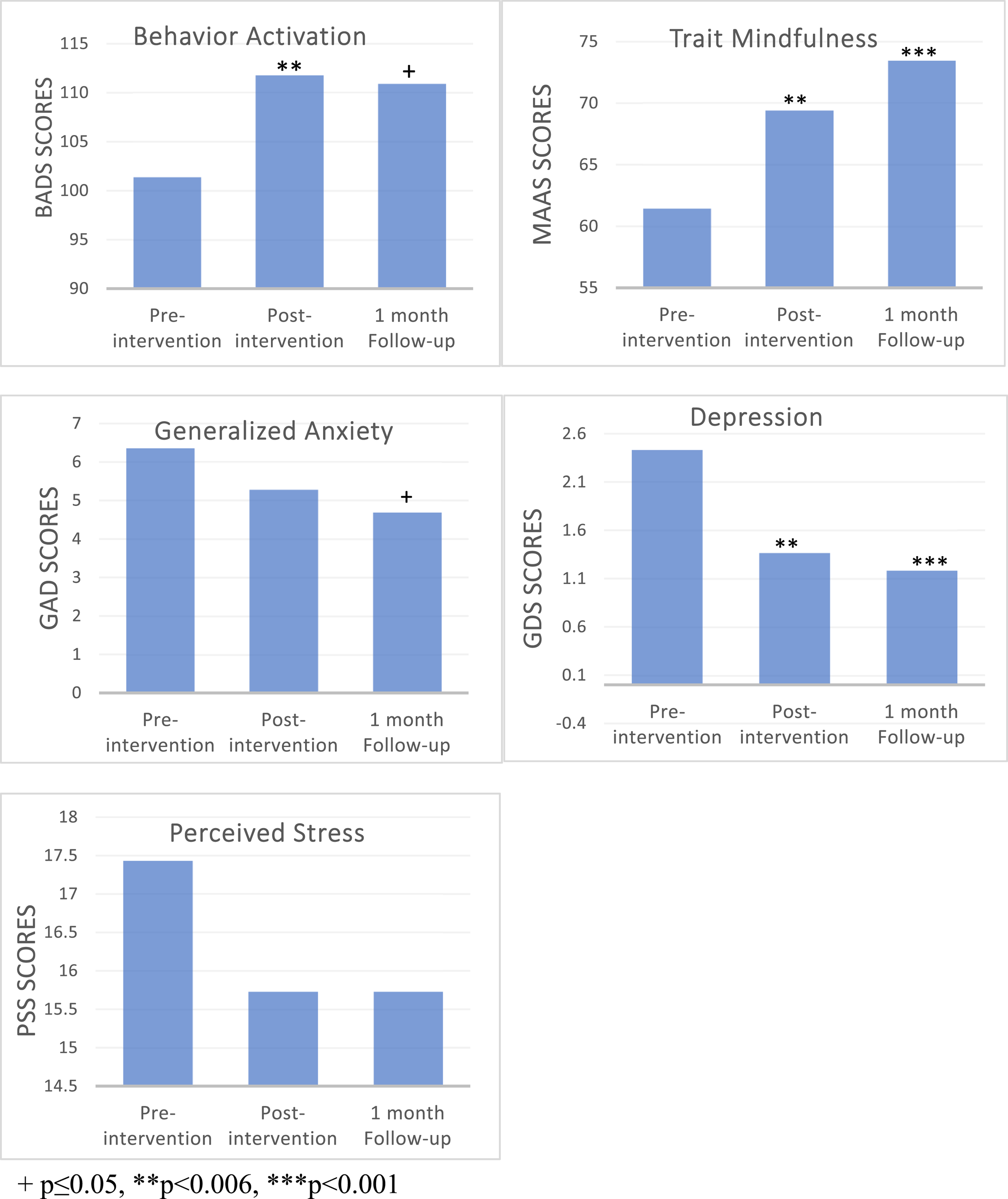
FIGURE 1. Psychological outcomes. +p ≤ 0.05, **p < 0.006, ***p < 0.001.
| N | Minimum | Maximum | Mean | Std. deviation | |
|---|---|---|---|---|---|
| GDS pre‐intervention | 28 | 0.00 | 7.00 | 2.43 | 1.85 |
| GDS post‐intervention | 22 | 0.00 | 4.00 | 1.36** | 1.33 |
| GDS follow‐up | 22 | 0.00 | 4.00 | 1.18*** | 1.22 |
| BADS pre‐intervention | 28 | 65.00 | 130.00 | 101.36 | 17.14 |
| BADS post‐intervention | 22 | 87.00 | 131.00 | 111.73** | 11.30 |
| BADS follow‐up | 22 | 80.00 | 137.00 | 110.85+ | 15.61 |
| MAAS pre‐intervention | 28 | 29.00 | 85.00 | 61.43 | 13.64 |
| MAAS post‐intervention | 22 | 51.00 | 90.00 | 69.36** | 11.03 |
| MAAS follow‐up | 22 | 45.00 | 89.00 | 73.41*** | 11.08 |
| GAD7 pre‐intervention | 28 | 1.00 | 17.00 | 6.36 | 3.85 |
| GAD7 post‐intervention | 22 | 0.00 | 11.00 | 5.27 | 2.85 |
| GAD7 follow‐up | 22 | 0.00 | 15.00 | 4.68+ | 3.92 |
| PSS pre‐intervention | 28 | 6.00 | 27.00 | 17.423 | 5.71 |
| PSS post‐intervention | 22 | 6.00 | 27.00 | 15.73 | 5.66 |
| PSS follow‐up | 22 | 6.00 | 28.00 | 15.73 | 5.86 |
Using linear‐mixed modeling, we found that BADS had a trend increase from pre‐intervention to post‐ (B = 8.58, t(26) = 2.29 p = 0.030) and significantly increased from pre‐intervention to 1‐month follow‐up B = 9.44, t(28) = 3.05 p = 0.005. The MAAS scores significantly increased from pre‐ to post‐intervention (B = 10.75, t(32) = 4.76 p < 0.001) and pre‐ to 1‐month follow‐up (B = 6.71, t(21) = 3.44 p = 0.002). The PSS score did not significantly change across any assessment.
DISCUSSION
Our aim for this study was to demonstrate the feasibility of using low‐cost, and minimally resource‐intensive VR‐delivered mindfulness in an older non‐English speaking sample in Ecuador—a low‐income country. We successfully demonstrated proof‐of‐concept for this approach, finding that it was acceptable, well tolerated, and with initial evidence of positive clinical impact. The attrition rate of this study was 21%, similar to that found in other mindfulness‐based interventions for older adults (19).
Furthermore, 17 participants (60%) had MCI, which is consistent with literature demonstrating that VR interventions can be deployed in this population (20, 21).
Although the absence of a control group limits our ability to determine if VR enhanced mindful states, we found that participants had significantly higher trait mindfulness scores post‐intervention and at 1‐month post‐intervention. It is possible that this finding represents the effect of more sustained attention to mindfulness tasks, as reported in studies in younger adults (22, 23, 24, 25). We noted that the intervention led to significant decreases in depression scores and increases in behavior activation scores. These results are both consistent with existing literature on the beneficial impact of mindfulness on mood (26, 27). In contrast, anxiety and perceived stress scores did not significantly change, which may be at least in part due to our participants' low baseline anxiety and stress scores (28).
Our study has several limitations. Our sample was one of convenience and biased towards those with access to social media. The absence of a control group, and a non‐clinical sample means that we cannot reliably infer the direct clinical impact of this intervention on symptoms. We also cannot quantify a differential impact from VR. A larger controlled study will need to replicate our findings and ascertain their generalizability. Additionally, the Sites in VR app used in this study necessitates a smartphone with a gyroscope, which is more expensive and may limit scalability to an extent. However, our approach represents a novel use of VR technology adapted for scaling to LMICs. This proof of concept along with a preliminary signal towards clinical efficacy has greater implications for how digital tools can be adapted for more equitable use globally. While our findings are modest, they are an important first step in this crucial direction.
Clinical Implications
Our study has clinical implications for older adults facing economic, language, and cultural barriers. Our results support the feasibility of broadening access and implementation of mindfulness interventions to diverse demographics. In essence, our findings suggest that VR‐delivered mindfulness interventions are a viable, accessible, and cost‐effective tool that could improve the well‐being and mental health of older adults, especially in resource‐limited settings.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28