History of Suicidality and Pandemic Outcomes: Longitudinal Associations with Anxiety Symptoms, Depressive Symptoms, and Problematic Drinking
Abstract
Objective
Individuals with a history of suicidality may be especially vulnerable to the adverse impact of COVID‐related stressors, but this vulnerability has not been demonstrated. This study examined the longitudinal effects of suicidality history (ideation only or attempt vs. none) and interactions with COVID‐related stressors (e.g., work interruptions, childcare challenges, and financial stress) on anxiety symptoms, depressive symptoms, and problematic drinking.
Methods
Longitudinal data from 517 participants were drawn from the National Institute on Alcohol Abuse and Alcoholism Natural History Protocol and COVID‐19 Pandemic Impact on Alcohol Study. Lifetime history of suicidality was assessed using the clinician administered Columbia‐Suicide Severity Rating Scale. Multiple regressions tested the interaction between suicidality history and COVID‐related stressors on clinical outcomes.
Results
Compared to individuals without any history of suicidality (79.9%; n = 413), individuals with a history of suicide ideation only (14.5%; n = 75) and suicide attempt (5.6%; n = 29) had higher anxiety symptoms, depressive symptoms, and problematic drinking during the pandemic. Significant interaction effects showed the associations between COVID‐related stressors and mental disorder symptoms were stronger among individuals with suicide attempt history than individuals without suicidality history.
Conclusions
History of suicide attempt in combination with high COVID‐related stressors put individuals at the greatest risk for pandemic mental disorder symptoms. Individuals with suicide attempt history may have lower coping resources to handle COVID‐related stressors. Suicide risk assessment and intervention to increase cognitive flexibility and emotional regulation skills may help these individuals manage emotional distress experienced during the COVID‐19 pandemic and beyond.
Highlights
Exposure to stress during the COVID‐19 pandemic is associated with worse mental disorder symptoms and higher problematic drinking. However, limited research has examined the potential role of suicidality history as a moderator of these associations.
In this longitudinal study, history of suicidality was assessed using the Columbia‐Suicide Severity Rating Scale and study participants were categorized into three groups: no history of suicidality, a history of suicide ideation only, and a history of suicide attempt.
Moderation analyses showed that exposure to pandemic stress was more strongly associated with mental disorder symptoms among individuals with a history of suicide attempt, suggesting the need to provide targeted interventions for this group.
Suicide is a major public health issue, with lifetime prevalence estimates of suicide ideation and attempt at 9.2% and 2.7%, respectively (1). At the start of the COVID‐19 pandemic, suicide researchers and public health experts predicted increased deaths by suicide amid a “perfect storm” of risk factors including isolation, financial distress, medical illness, and barriers to treatment (2, 3). While deaths by suicide were either unchanged or declined in parts of the U.S. during the initial phase of the COVID‐19 pandemic (4), several meta‐analyses have found increased rates of suicide ideation and attempts (5, 6). This increase is of significant clinical concern, as lifetime suicide ideation and/or attempts are associated with later disability estimates and reduced physical/psychological quality of life (7, 8).
In a meta‐analytic review, a myriad of risk factors was identified as correlates of suicide ideation during the COVID‐19 pandemic, including quarantine and exhaustion, low social support, sleep disturbances, loneliness, and mental health difficulties (9). COVID‐related experiences such as the impact of social distancing policies and fear of physical harm have also been linked to past‐month suicidal ideation and suicide attempt among U.S. adults (10). Although these studies provided cross‐sectional evidence connecting COVID‐related stressors and emotional distress during the pandemic to suicide ideation, limited research has utilized longitudinal data to examine if a history of suicidality may be associated with mental disorder symptoms and problematic drinking in the context of the COVID‐19 pandemic.
During the first year of the COVID‐19 pandemic, anxiety and depression increased by 25% and alcohol‐related mortality also increased by 25% (11, 12). These increases may be attributable to social isolation during the initial phase of the pandemic (13), and exposure to COVID‐related stressors such as disruption to employment and financial stress over the course of the pandemic (14). Worsened depression and anxiety symptoms have been especially pronounced among those who use avoidance coping strategies such as denial, venting, and behavioral disengagement (15), which may trigger drinking alcohol to cope with pandemic stress (16). Global rates of depressive and anxiety symptoms increased since the start of the COVID‐19 pandemic (17), with adverse outcomes particularly elevated among those reporting COVID‐19 stressors (18).
A meta‐analytic review of 128 studies examining changes in alcohol consumption during the first year of the COVID‐19 pandemic showed substantial heterogeneity in drinking patterns (19). A wide range of risk factors was summarized in this meta‐analysis, including income loss, working remotely, and mental health issues such as depression, but a history of suicidality was not listed as a distinct risk factor. Furthermore, during the pandemic, individuals may engage in problematic drinking as a maladaptive coping strategy to manage and reduce symptoms of depression, anxiety, and other acute stressors (20, 21). Despite these studies, it is unclear whether the adverse effects of COVID‐related stressors on mental disorder symptoms and problematic drinking are stronger among those with a history of suicidality.
This study had two goals. First, we investigated the longitudinal associations of history of suicide ideation and attempt with depressive symptoms, anxiety symptoms, and problematic drinking. Second, we examined if the association of COVID‐related stressors and clinical outcomes were moderated by history of suicidality. Recent research has emphasized the importance of distinguishing between clinical characteristics among individuals with suicide attempt versus ideation only (22). We hypothesized that individuals with a history of suicide attempt would report the highest levels of mental disorder symptoms and problematic drinking, followed by individuals with a history of suicide ideation only and then by individuals without any history of suicidality. We also hypothesized that the magnitude of associations between COVID‐related stressors and clinical outcomes would be stronger among individuals with a history of suicide ideation and/or attempt compared to those without any history of suicidality.
METHOD
Participants
From June 3, 2020 to January 19, 2023, 589 adults were enrolled in the National Institute on Alcohol Abuse and Alcoholism (NIAAA) COVID‐19 Pandemic Impact on Alcohol Study (C19 PIA Study). These participants were previously enrolled in the NIAAA Natural History Protocol (NHP), from which data on history of suicidality and alcohol use disorder (AUD) diagnosis were gathered through clinical interviews. The identification of study participants was based on contact information collected in the NHP and recruitment of participants was completed over the phone by trained clinical interviewers. As shown in Figure 1, we excluded 71 participants with missing data on one or more key study measures and 1 participant who completed the NHP and C19 PIA Study assessments on the same day, yielding an analytic sample of 517 participants (87.8% of the larger sample of 589 adults in the C19 PIA Study). For all participants, their assessment in the C19 PIA Study was at least 1 week after their assessment in the NHP. As described below, this design‐related variation was statistically adjusted for using the cohort variable. At the time of the C19 PIA Study, 86.5% of participants resided in the Washington metropolitan region (59.0% Maryland; 11.6% Virginia; 15.9% Washington, DC). All participants provided informed consent before they were enrolled in the C19 PIA Study. Verbal consent and C19 PIA Study assessments on COVID‐related stressors and clinical outcomes were obtained over the phone. The C19 PIA Study protocol was approved by the NIH Intramural Institutional Review Board and has been registered in clinicaltrials.gov (NCT04391816).
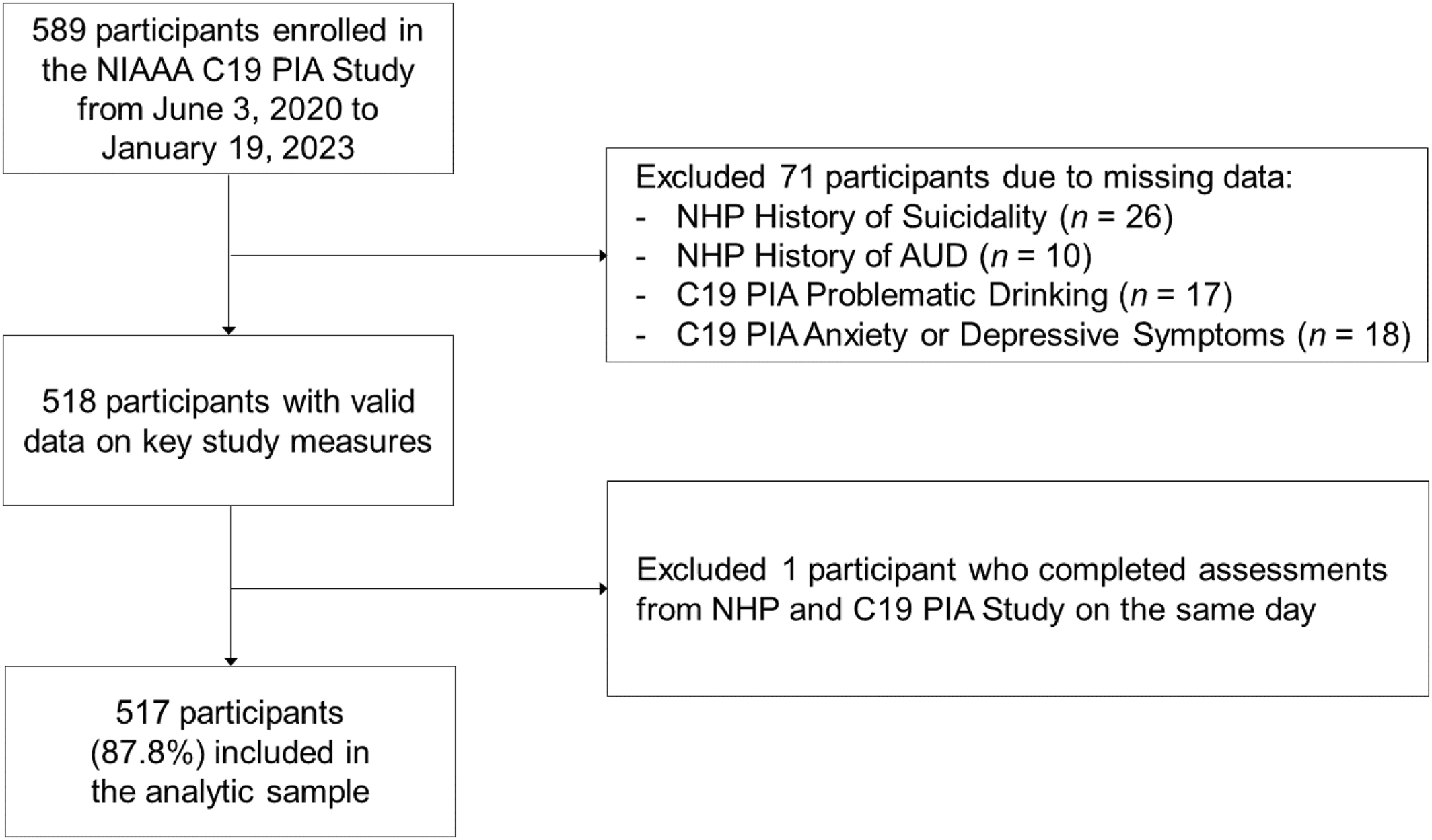
FIGURE 1. Flow diagram illustrating participation inclusion and exclusion.
Measures
History of Suicidality (NHP)
Lifetime history of suicide ideation and attempt was assessed using the clinician administered Columbia‐Suicide Severity Rating Scale (C‐SSRS) (23). Three items on passive suicide ideation, active suicide ideation, and suicide attempt were used to categorize participants into three groups: (1) 413 with no history of suicidality (79.9%), (2) 75 with suicide ideation history only (14.5%), and (3) 29 with suicide attempt history (5.6%). All response pattern combinations are detailed in Table S1.
History of AUD (NHP)
AUD diagnosis was assessed using the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV or DSM‐5) administered by trained clinicians (24).
COVID‐Related Stressors (C19 PIA)
Participants were asked “How has the COVID‐19 outbreak affected you?” Seventeen items derived from the COVID‐19 Community Survey Question Bank assessed the impact of COVID‐19 on work, childcare, finances, living condition, and health of family or friends (14, 25). The wording of these items along with endorsement frequencies and percentages are presented in Table S2. After reverse coding two positively phrased items, a total score was used to indicate COVID‐related stress (Cronbach's α = 0.71).
Anxiety Symptoms (C19 PIA)
Anxiety symptoms in the past month were assessed using the Generalized Anxiety Disorder‐7 (GAD‐7) assessment (26). The GAD‐7 has 7 items ranging from 0 to 3 and has a maximum total score of 21 (Cronbach's α = 0.92).
Depressive Symptoms (C19 PIA)
Depressive symptoms in the past month were assessed using the Patient Health Questionnaire (PHQ‐9) assessment (27). The PHQ‐9 has 9 items ranging from 0 to 3 and has a maximum total score of 27 (Cronbach's α = 0.88).
Problematic Drinking (C19 PIA)
Problematic drinking in the past year was assessed using the 10‐item Alcohol Use Disorders Identification Test developed by the World Health Organization (28). Each item responses ranged from 0 to 4, yielding a maximum total score of 40 (Cronbach's α = 0.94).
Design‐Related Covariates
Two study design related issues were addressed by including the following covariates. First, time lapsed from the NHP to the C19 PIA Study varied across participants, with a mean of 684 days (median = 475 days; range = 8–2290 days). To control for this variation, we coded time lapsed into a cohort variable with four categories: <1 year (44.7%), 1 year (16.4%), 2–3 years (22.1%), and 4 or more years (16.8%). Second, as participants were enrolled into the C19 PIA Study on a rolling basis, there were variations in COVID‐19 infection rates, local government policies, and availability of vaccination across time. To control for this variation, we coded timing of enrollment into an enrollment phase variable with five categories: Phase 1 (June 3, 2020 to July 31, 2020; 19.9%), Phase 2 (August 1, 2020 to November 22, 2020; 25.2%), Phase 3 (November 23, 2020 to Feb 28, 2021; 23.6%), Phase 4 (March 1, 2021 to November 31, 2021; 14.3%), and Phase 5 (December 1, 2021 to January 19, 2023; 17.0%).
Statistical Analyses
We conducted the statistical analyses in three steps. First, chi‐square and one‐way analysis of variance tests were conducted to compare differences in sample characteristics and study variables across the three history of suicidality groups. Significant differences were probed using follow‐up multinomial logistic regressions (for categorical variables) and pairwise comparisons with the Bonferroni adjustment (for continuous variables). Second, three linear regression models were specified to examine the associations of history of suicidality with anxiety symptoms, depressive symptoms, and problematic drinking. Third, the interactions between COVID‐related stressors and history of suicidality were investigated in three multiple regression models that covaried for cohort, enrollment phase, age, sex, race, ethnicity, marital status, and history of AUD. To probe any significant interactions, the simple slopes of COVID‐related stressors on clinical outcomes were estimated. For any model with nonsignificant interactions, the final model would be re‐estimated without the interaction terms. All statistical analyses were conducted in Stata 17.
RESULTS
Table 1 shows sample characteristics and study variables for the overall sample and by history of suicidality groups. Chi‐square tests revealed differences in sex, race, and history of AUD by history of suicidality groups, and follow‐up multinomial logistic regressions were conducted. Male participants were marginally less likely than female participants to endorse a history of suicide attempt (p = 0.062). Relative to White participants, Black/African American participants were less likely to endorse a history of suicide ideation (p = 0.004). History of AUD was strongly associated with history of suicide ideation and attempt. Relative to those without a history of AUD, individuals with a history of AUD were much more likely to endorse a history of suicide ideation only (70.7% vs. 31.5%; p < 0.001) or a history of suicide attempt (82.8% vs. 31.5%; p < 0.001). One‐way ANOVAs showed significant suicidality history group differences in COVID‐related stressors and clinical outcomes, in which individuals with a history of either suicide ideation only or suicide attempt reported elevated scores compared to those without any history of suicidality.
| Overall sample (N = 517) | None (n = 413) | Suicide ideation only (n = 75) | Suicide attempt (n = 29) | χ2 | p | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |||
| Sex | ||||||||||
| Female | 242 | 46.8 | 195 | 47.2 | 28 | 37.3 | 19 | 65.5 | 6.81 | 0.033 |
| Male | 275 | 53.2 | 218 | 52.8 | 47 | 62.7 | 10 | 34.5 | ||
| Race | ||||||||||
| White | 263 | 50.9 | 202 | 48.9 | 49 | 65.3 | 12 | 41.4 | 10.52 | 0.033b |
| Black/African American | 174 | 33.7 | 147 | 35.6 | 14 | 18.7 | 13 | 44.8 | ||
| Other | 80 | 15.5 | 64 | 15.5 | 12 | 16.0 | 4 | 13.8 | ||
| Ethnicity | ||||||||||
| Not Hispanic | 454 | 87.8 | 363 | 87.9 | 66 | 88.0 | 25 | 86.2 | 2.33 | 0.676 |
| Hispanic | 43 | 8.3 | 32 | 7.8 | 8 | 10.7 | 3 | 10.3 | ||
| Unknown | 20 | 3.9 | 18 | 4.4 | 1 | 1.3 | 1 | 3.5 | ||
| Marital status | ||||||||||
| Single | 331 | 64.0 | 265 | 64.2 | 47 | 62.7 | 19 | 65.5 | 2.17 | 0.705 |
| Married | 106 | 20.5 | 88 | 21.3 | 14 | 18.7 | 4 | 13.8 | ||
| Other | 80 | 15.5 | 60 | 14.5 | 14 | 18.7 | 6 | 20.7 | ||
| History of AUD | ||||||||||
| No | 310 | 60.0 | 283 | 68.5 | 22 | 29.3 | 5 | 17.2 | 63.96 | <0.001 |
| Yes | 207 | 40.0 | 130 | 31.5 | 53 | 70.7 | 24 | 82.8 | ||
| M | SD | M | SD | M | SD | M | SD | F | p | |
| Age | 44.59 | 14.13 | 44.43 | 14.33 | 43.91 | 13.30 | 48.69 | 13.22 | 1.34 | 0.263 |
| COVID stressors | 3.82 | 2.69 | 3.73 | 2.71 | 4.13 | 2.58 | 4.38 | 2.69 | 1.37 | 0.254 |
| Anxiety symptoms | 4.33 | 5.02 | 3.75 | 4.66 | 6.80 | 5.87 | 6.28 | 5.40 | 14.77 | <0.001c |
| Depressive symptoms | 4.76 | 5.55 | 3.97 | 4.97 | 7.71 | 6.35 | 8.34 | 7.20 | 22.58 | <0.001c |
| Problematic drinking | 8.67 | 11.04 | 7.13 | 9.89 | 15.21 | 13.08 | 13.55 | 13.34 | 21.63 | <0.001c |
Figure 2 illustrates the longitudinal associations of suicidality history with anxiety symptoms, depressive symptoms, and problematic drinking. Results from linear regression models showed that relative to individuals without any history of suicidality, those with a history of suicide ideation only reported higher anxiety symptoms (b = 3.05, 95% CI = 1.85, 4.26, p < 0.001), depressive symptoms (b = 3.74, 95% CI = 2.42, 5.05, p < 0.001), and problematic drinking (b = 8.08, 95% CI = 5.46, 10.70, p < 0.001). Similarly, individuals with a history of suicide attempt also reported higher anxiety symptoms (b = 2.53, 95% CI = 0.68, 4.37, p = 0.007), depressive symptoms (b = 4.38, 95% CI = 2.36, 6.39, p < 0.001), and problematic drinking (b = 6.42, 95% CI = 2.41, 10.43, p = 0.002).
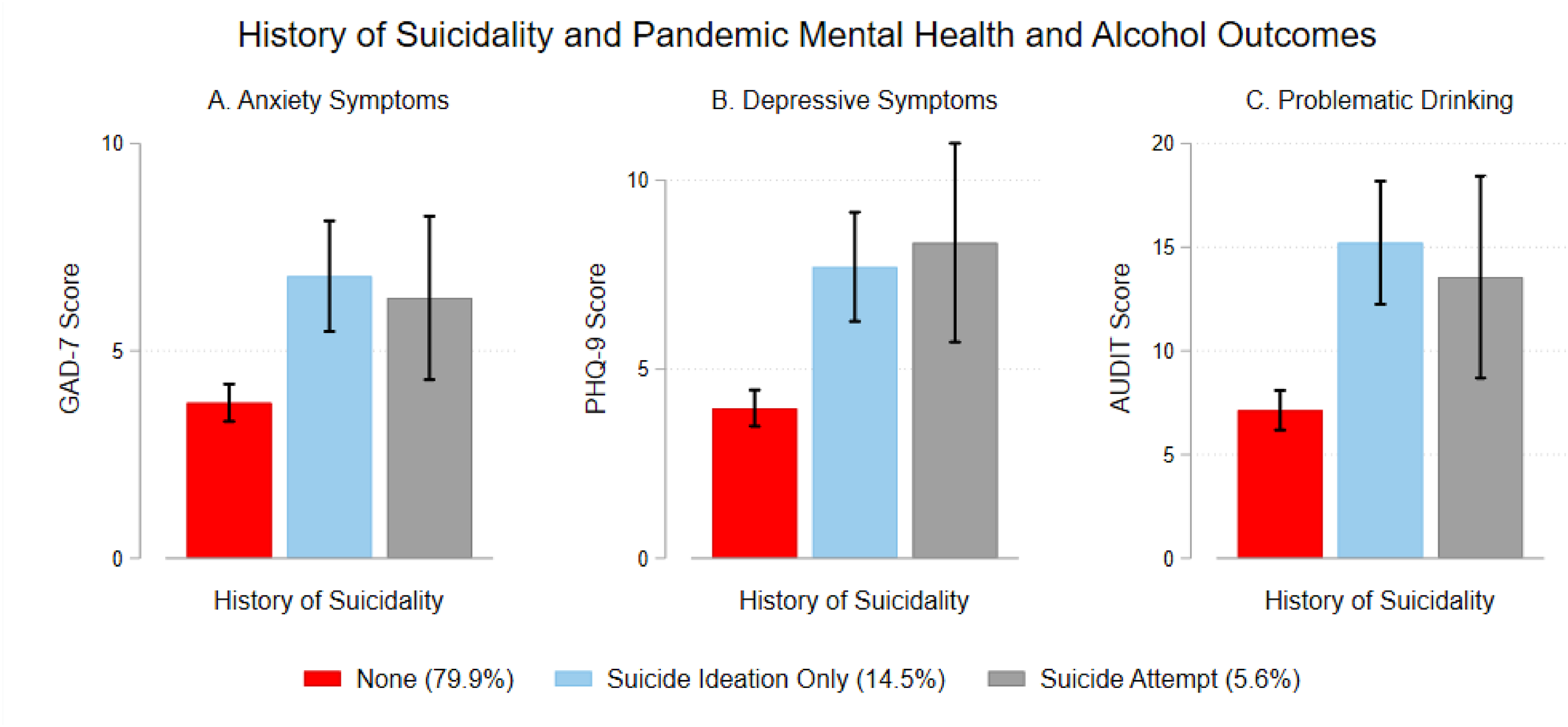
FIGURE 2. Longitudinal impact of history of suicidality on anxiety symptoms, depressive symptoms, and problematic drinking. Compared to those who had no history of suicidality, individuals who had a history of suicide ideation or attempt reported higher levels of anxiety symptoms, depressive symptoms, and problematic drinking. Error bars represent 95% confidence intervals.
Table 2 shows the multiple regression models testing the interaction between COVID‐related stressors and history of suicidality on mental disorder symptoms and problematic drinking. The interaction between COVID‐related stressors and history of suicide attempt was significant for anxiety symptoms (b = 0.92, 95% CI = 0.24, 1.60, p = 0.008) and depressive symptoms (b = 1.03, 95% CI = 0.29, 1.76, p = 0.006). As shown in Table S3, the simple slopes of COVID‐related stressors on mental disorder symptoms were significant among individuals without any history of suicidality (b = 0.28, 95% CI = 0.10, 0.46, p = 0.002 for anxiety symptoms; b = 0.32, 95% CI = 0.12, 0.51, p = 0.001 for depressive symptoms), and the magnitudes of these associations were substantially stronger among individuals with a history of suicide attempt (b = 1.20, 95% CI = 0.55, 1.85, p < 0.001 for anxiety symptoms; b = 1.34, 95% CI = 0.64, 2.05, p < 0.001 for depressive symptoms). These interaction effects are visually illustrated in Figure 3. Of note, due to relatively few participants in the history of suicide attempt group (n = 29), the 95% CI bounds were wider for this group. As for problematic drinking, history of AUD was strongly associated with problematic drinking. COVID‐related stressors and later enrollment phases were also positively associated with problematic drinking. When the nonsignificant interaction terms were dropped in the final multiple regression model, history of suicide ideation was positively associated with problematic drinking (b = 2.87, 95% CI = 0.75, 4.99, p = 0.008), whereas history of suicide attempt was not associated with problematic drinking (b = 0.58, 95% CI = −2.64, 3.79, p = 0.724).
| Anxiety symptoms | Depressive symptoms | Problematic drinking | |||||||
|---|---|---|---|---|---|---|---|---|---|
| b | SE | p | b | SE | p | b | SE | p | |
| Intercept | 4.02 | 0.92 | <0.001 | 4.79 | 1.00 | <0.001 | 1.02 | 1.61 | 0.526 |
| COVID‐related stressors | 0.28 | 0.09 | 0.002 | 0.32 | 0.10 | 0.001 | 0.44 | 0.16 | 0.005 |
| History of suicidality | |||||||||
| Ideation versus none | 1.62 | 1.13 | 0.151 | 2.96 | 1.22 | 0.016 | 0.36 | 1.97 | 0.854 |
| Attempt versus none | −2.60 | 1.78 | 0.145 | −1.48 | 1.94 | 0.445 | 3.78 | 3.11 | 0.225 |
| Interactions | |||||||||
| COVID‐related stressors × ideation | 0.11 | 0.23 | 0.622 | −0.07 | 0.25 | 0.786 | 0.61 | 0.40 | 0.130 |
| COVID‐related stressors × attempt | 0.92 | 0.34 | 0.008 | 1.03 | 0.37 | 0.006 | −0.72 | 0.60 | 0.233 |
| Enrollment phase | |||||||||
| 2 versus 1 | 0.47 | 0.73 | 0.521 | −0.21 | 0.80 | 0.793 | 0.59 | 1.28 | 0.647 |
| 3 versus 1 | 0.34 | 0.73 | 0.647 | −0.27 | 0.79 | 0.737 | 3.66 | 1.28 | 0.004 |
| 4 versus 1 | 0.81 | 0.75 | 0.280 | 0.32 | 0.82 | 0.697 | 5.37 | 1.31 | <0.001 |
| 5 versus 1 | −0.35 | 0.71 | 0.623 | −0.26 | 0.77 | 0.737 | 3.36 | 1.24 | 0.007 |
| Cohort | |||||||||
| 1 year versus <1 year | 1.65 | 0.72 | 0.023 | 2.26 | 0.79 | 0.004 | −1.50 | 1.26 | 0.235 |
| 2–3 years versus <1 year | 0.60 | 0.71 | 0.403 | 1.48 | 0.77 | 0.056 | −2.93 | 1.24 | 0.019 |
| 4+ years versus <1 year | −1.02 | 0.72 | 0.160 | −0.34 | 0.79 | 0.670 | −4.19 | 1.26 | 0.001 |
| Age | −0.04 | 0.02 | 0.028 | −0.05 | 0.02 | 0.004 | −0.01 | 0.03 | 0.846 |
| Sex | |||||||||
| Male versus female | −0.22 | 0.43 | 0.609 | −0.53 | 0.46 | 0.252 | 0.17 | 0.75 | 0.824 |
| Race | |||||||||
| Black/African versus White | −0.57 | 0.48 | 0.230 | −0.70 | 0.52 | 0.175 | −1.59 | 0.83 | 0.057 |
| Other versus White | −0.31 | 0.65 | 0.633 | −0.92 | 0.70 | 0.193 | −2.26 | 1.13 | 0.047 |
| Hispanic | |||||||||
| Hispanic versus non‐Hispanic | −0.53 | 0.80 | 0.507 | −0.47 | 0.86 | 0.585 | 2.10 | 1.39 | 0.130 |
| Unknown versus non‐Hispanic | −0.67 | 1.10 | 0.546 | −0.70 | 1.20 | 0.560 | 3.24 | 1.93 | 0.093 |
| Marital status | |||||||||
| Married versus single | −0.75 | 0.56 | 0.177 | −0.68 | 0.60 | 0.261 | 0.60 | 0.97 | 0.534 |
| Other versus single | −0.80 | 0.63 | 0.204 | 0.87 | 0.69 | 0.207 | 2.71 | 1.10 | 0.014 |
| History of AUD | 1.70 | 0.48 | <0.001 | 1.79 | 0.52 | 0.001 | 12.34 | 0.84 | <0.001 |
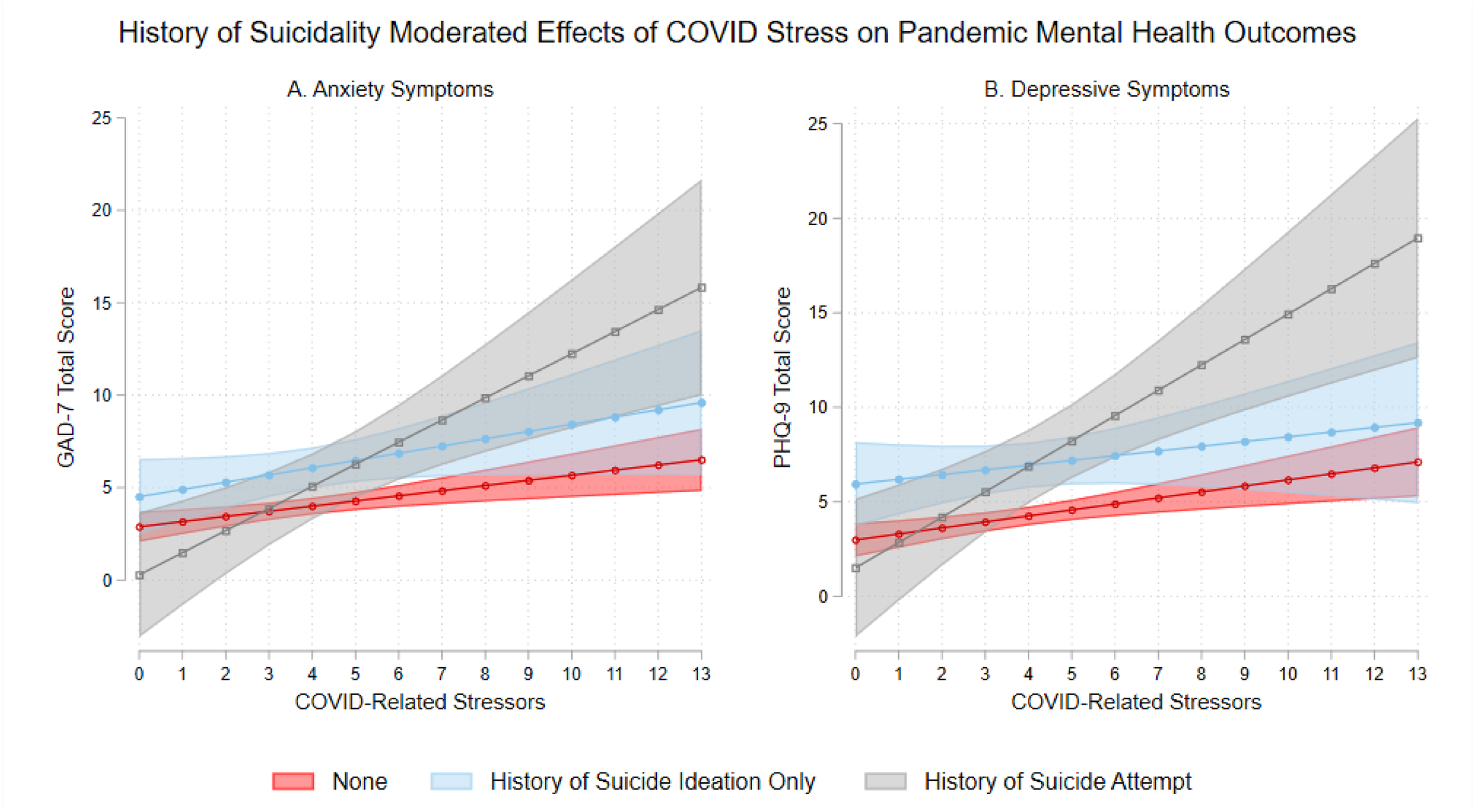
FIGURE 3. Interactions between COVID‐related stressors and history of suicidality on anxiety and depressive symptoms. COVID‐related stressors were positively associated with both anxiety and depressive symptoms, and especially so for those with a history of suicide attempt. Shaded areas represent 95% confidence intervals.
DISCUSSION
Extending cross‐sectional studies that connected mental disorder symptoms to suicide ideation and attempt during the COVID‐19 pandemic (9, 29), the current study showed longitudinal associations of a history of suicide ideation and/or attempt with higher depression symptoms, anxiety symptoms, and problematic drinking during the pandemic. While mental disorder symptoms and problematic drinking were generally higher among individuals with a history of suicide ideation or attempt than those without, contrary to our hypothesis, a history of suicide attempt was not associated with the highest levels of symptomology. Prior research showed that higher acquired capability to attempt suicide and negative urgency were particularly elevated among individuals with suicide attempt history versus ideation history only (22, 30). It is possible that differences between individuals with suicide attempt history and ideation history only are manifested not across a broad spectrum of clinical characteristics, but only to specific vulnerability factors that are most closely linked to suicide attempt. Overall, the current findings highlight a history of suicide ideation and/or attempt as a risk indicator for mental disorder symptoms and maladaptive drinking to cope during the pandemic and reinforce the importance of continued surveillance and prevention of adverse suicide‐related consequences over time (3). The novel interaction findings help inform who may need intervention, which is consistent with stress sensitization models that suggest a history of adversity, such as suicidality history, may increase vulnerability for the development of mental health concerns in response to stressful events (31). Moreover, as the majority (>80%) of participants with suicide attempt also had a history of AUD, our findings suggest the need to assess and treat alcohol misuse in the context of suicide prevention.
Within this sample, the associations between COVID‐related stressors and mental disorder symptoms were stronger among individuals with a history of suicide attempt than individuals without a history of suicidality. This finding may reflect differences in emotion regulation and use of adaptive coping strategies in response to COVID‐related stressors. Research suggests difficulties in emotion regulation, including nonacceptance of emotional distress and perceived lack of access to effective emotion regulation strategies, were associated with greater COVID‐19 related acute stress (32). Furthermore, adaptive emotion regulation strategies, such as cognitive reappraisal, served as a buffer between COVID‐19 related stress and increased mental distress, whereas maladaptive emotion regulation strategies, such as suppression, exacerbated the association between COVID‐19 related stress and increased general mental distress (33). In line with these prior findings, individuals with a history of suicide attempt may be more vulnerable to the impact of COVID‐related stressors on anxiety and depressive symptoms due to greater emotion dysregulation and lower use of adaptive coping strategies. These findings are relevant to clinical care as suicide risk assessment has been proposed as an important clinical pathway in primary care settings and in mental health clinics (34, 35). More research is needed to test these potential mechanisms and develop interventions to help individuals with a history of suicide attempt develop adaptive coping and emotion regulation skills.
In this study, individuals with a history of suicide ideation and/or attempt generally reported higher problematic drinking, which is consistent with studies completed prior to the COVID‐19 pandemic (36). However, after adjusting for covariates such as COVID‐related stressors and a history of AUD, the associations of a history of suicide ideation and/or attempt with problematic drinking were attenuated. These findings may reflect the significant role of COVID‐related stressors in problematic drinking during the pandemic (14, 16), and the substantial overlap between history of AUD and suicidality (37, 38). Remarkably, in the current sample, 31.5% of individuals without history of suicidality met criteria for AUD, whereas 70.7% of individuals with suicide ideation and 82.8% of individuals with suicide attempt met criteria for AUD. Recent research has sought to better understand the overlap between suicide‐related and addictive behaviors and develop integrative intervention approaches for this population (39). More research is needed to study common etiological factors such as impulsivity and emotional dysregulation that characterize individuals with both AUD and suicide‐related behaviors. A better understanding of shared etiological pathways leading to this comorbidity can inform optimal intervention strategies that address the unique needs of this underserved population.
Despite its novelty, including the differentiation between suicide attempt history versus ideation history only and the longitudinal analyses with multiple clinical outcomes, this study has several limitations. First, while history of suicidality was assessed by clinicians in the NHP, all outcome measures assessed during the pandemic were based on self‐report and may be susceptible to recall bias. Second, the C19 PIA Study recruited participants on a rolling basis and so the baseline assessment may reflect different phases of the pandemic. While we statistically adjusted for this variation in our analyses, variations in COVID‐related policies and other pandemic‐related factors may still have played a role in participants' mental disorder symptoms and problematic drinking. Third, participant identification and recruitment were restricted to prior participants in the NHP who primarily resided in the Washington metropolitan region. Given the use of a regional sample, the findings from the current study may not be generalizable to individuals living in other states or to populations that are dissimilar to the demographic makeup of the study sample. Fourth, there were relatively few participants with a history of suicide attempt (n = 29) and so the estimates were less precise as indicated by the wider 95% confidence intervals. Finally, C‐SSRS was only administered in the NHP and current suicide ideation, plan, and attempt were not evaluated during the pandemic. Thus, the available data did not allow for the examination of how change in suicide ideation and/or attempt may be associated with change in psychological distress and problematic drinking. Despite this caveat, the availability of clinician‐administered C‐SSRS data is a unique strength of this study.
In conclusion, in this longitudinal investigation, a history of suicidality was associated with pandemic outcomes including anxiety symptoms, depressive symptoms, and problematic drinking. Uniquely, we identified individuals with a history of suicide attempt as a distinct group of individuals whose mental disorder symptoms were particularly vulnerable to the adverse impact of COVID‐related stressors. Clinically, the utilization of in‐person and distance‐based suicide prevention strategies to address concerns related to economic stress, social isolation, decreased social support, and barriers to mental health treatment should be considered as ways to reduce burden associated with mental health issues and suicidality (2). Individuals with a history of suicidality, and especially those with a history of suicide attempt, may benefit from interventions that promote emotional regulation skills and cognitive flexibility during a time of significant stress exposure (40). Improved coping skills and resources may help these individuals better manage suicide risk and related mental disorder symptoms in face of heightened stress amidst the pandemic and beyond.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40